Please click on the tables and figures to enlarge
Improving the awareness of carbon emissions from nitrous oxide use for patients receiving inhalation sedation
R. Lee*1, BDS BSc MFDS RCS (Eng) AKC
Z. Shehabi2, BDS MFDS MSc (SSCD) MSCD MSc (Healthcare management)
1Dental Core Trainee 1 in General Duties & Oral & Maxillofacial Surgery, The Royal London Dental Hospital, Turner Street, London, E1 1FR
2Clinical Lead and Consultant in Special Care Dentistry, The Royal London Dental Hospital, Turner Street, London, E1 1FR
*Correspondence to: R. Lee
Email: ronan.lee1@nhs.net
Lee R, Shehabi Z. Improving the awareness of carbon emissions from nitrous oxide use for patients receiving inhalation sedation . SAAD Dig. 2025: 41(I): 50-61
Abstract
Background
Nitrous oxide () with oxygen is a safe and effective conscious sedation drug. However, N2O is a potent greenhouse gas, 300 times more harmful than carbon dioxide. Despite a nationwide push to decommission N2O from NHS gas manifolds, there is limited data on its justified use in dentistry.
Aims
The project aimed to quantitatively record carbon emissions, time of N2O use, and evaluate success and justification. The secondary aim was to qualitatively assess N2O use, stored and to assess clinician's views of N2O use.
Method
This project collected quantitative data over three retrospective months (May– July 2023), and one prospective month (January 2024), after implementing changes in the Special Care and Paediatric department. Qualitative data were collected from clinicians on N2O storage and use along with feedback.
Results / discussion
The results highlight the consistent justification for using N2O for inhalation sedation, as well as its success rate in achieving effective sedation, both retrospectively and prospectively across both departments. Improved recording of N2O usage time was observed following procedural changes. Prospective data highlighted higher carbon emissions in the paediatric department. Storage spot checks revealed proper procedures, but labelling discrepancies. Clinicians demonstrated safe practice, unanimous support for increased environmental awareness, and strong opposition to decommissioning of N2O. Recommendations and emphasis on sustainable N2O practice and environmental awareness were highlighted.
Key learning points
- This quality improvement project demonstrates consistent justification and effective nitrous oxide (N2O) use in both paediatric and special care departments
- The implementation of a new proforma for recording the time of N2O usage significantly improved the accuracy of carbon emission calculations in both departments
- There is consensus amongst dental clinicians for increased awareness regarding the environmental impact of N2O through an expressed commitment to sustainable practice.
Background
Nitrous oxide (N2O) in combination with oxygen (O2) is predominantly used as an inhaled gas for dental conscious sedation, defined as, ‘the technique that produces a state of central nervous system depression to enable treatment to be delivered but during which level contact with the patient is maintained throughout the period of sedation’.1,2 Inhalation sedation (IHS) aims to induce anxiolysis, alleviate fear and improve patient co-operation, ultimately facilitating dental treatment. N2O is a weak anaesthetic gas, with both sedative and pain relief properties, and is suitable for both adults and children as a safe and effective form of conscious sedation.2,3 N2O and O2 are delivered via a nasal hood placed over the patient’s nose. Once inhaled, N2O is expired into the environment via the lungs virtually unchanged, with trace amounts metabolised through reduction by gut bacteria.4
The success of N2O is dependent on its appropriate titration, and support by non-pharmacological behavioural management techniques. With proper case selection, N2O can achieve high success rates ranging between 93.6 to 94.9.%.5,6 While systematic reviews report a higher success rate amongst adults (99%) than children (91.9%),6 some studies suggest a lower success rate, especially for children with more complex needs who otherwise require treatment under general anaesthetic (GA).7 Nevertheless, IHS remains an effective and safe option for many patients.
N2O is used to manage a broad spectrum of children and adults with dental anxiety; gag reflex; medical conditions that compromise patients; prophylactically to prevent medical emergencies; and those who are undergoing long unpleasant procedures.8 However, it may not be appropriate for patients with severe respiratory infection / disease, patients with nose blockages, some patients undergoing ocular procedures and pre- / unco- operative patients. Alternative options to IHS include the use of intravenous sedation (IVS) or GA which have their limitations including age restrictions, increased risk of complications and limited access,2 furthermore, the use of GA requires more resources (ventilation of theatres, staff, consumables etc) which may result in higher carbon emissions when contrasted with IHS or IVS.9
Environmental impact
A caveat of N2O is that it is a potent greenhouse gas, approximately 300 times more harmful to the environment than carbon dioxide (CO2).10 Over the past 150 years, the increasing atmospheric concentration of N2O has contributed to the depletion of the ozone layer and climate change.11,12 In the National Health Service (NHS), anaesthetic gases including N2O make up to 5% of the total NHS carbon footprint.9 Concerning dentistry, research by Public Health England found N2O makes up 0.9% of the total NHS dental carbon footprint, and between 80 to 90% of the carbon footprint for a single procedure.13 N2O can be supplied either via mobile cylinders or piped connected to a central manifold within a building, the advantages and disadvantages of which can be seen in Table 1. Emerging evidence suggests that N2O wastage from piped manifold systems is a major contributor to the anaesthetic carbon footprint, estimating an annual wastage of 13.7 million litres of N2O across the UK and Ireland.14 At the Royal London Dental Hospital (RLDH), N2O is supplied in free-standing 1800L Size E Medical grade N2O cylinders supplied by BOC™.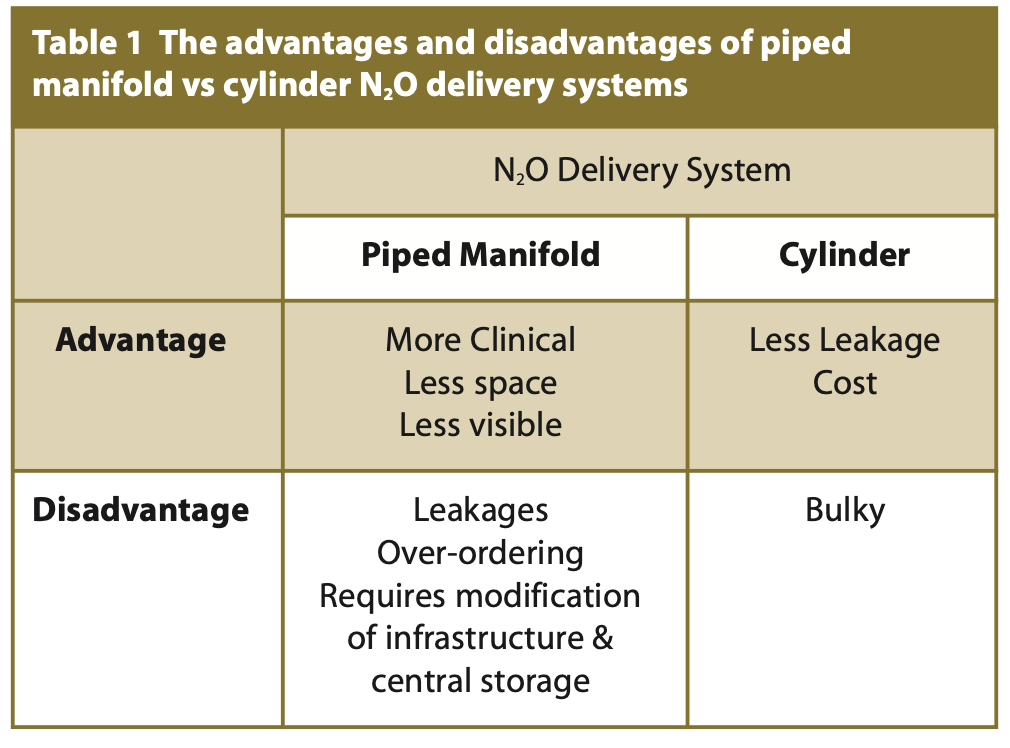
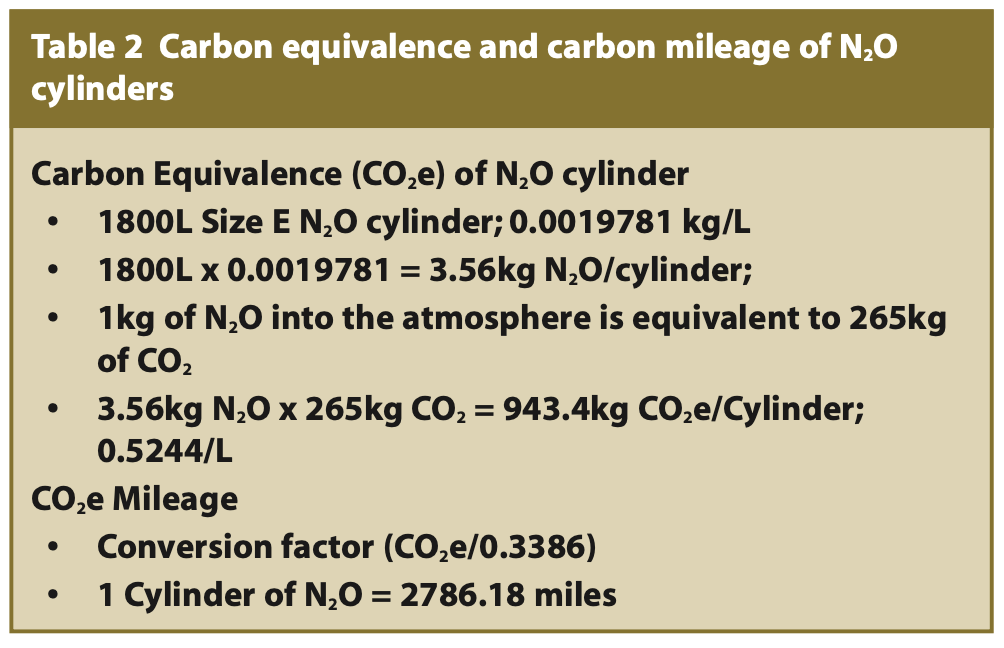
To assess the carbon emissions, a metric used to express the global warming potential of greenhouse gases in terms of their equivalence to CO2 termed ‘carbon equivalence’ (CO2e) and CO2e mileage can be calculated (see Table 2).15 When utilising N2O, an estimated 1.875kg/m3 of N2O equates to 3.375kg N2O per cylinder, and roughly 0.3068kg N2O per patient session. This results in a CO2e of roughly 91.43, equivalent to driving 30.9 miles.16 BOC™ data from 2019/2020, found that piped manifold N2O and Entonox® produced up to 27% and 45% of the anaesthetic emissions for NHS England respectively.17 While there has been a nationwide initiative to decommission N2O from NHS gas manifolds, limited data exists on the utilisation and justification of N2O in dentistry.9 Recording carbon emissions per N2O treatment session offers an opportunity to quantify N2O use and implement mitigation strategies to contribute to the Net Zero NHS target by 2040.9
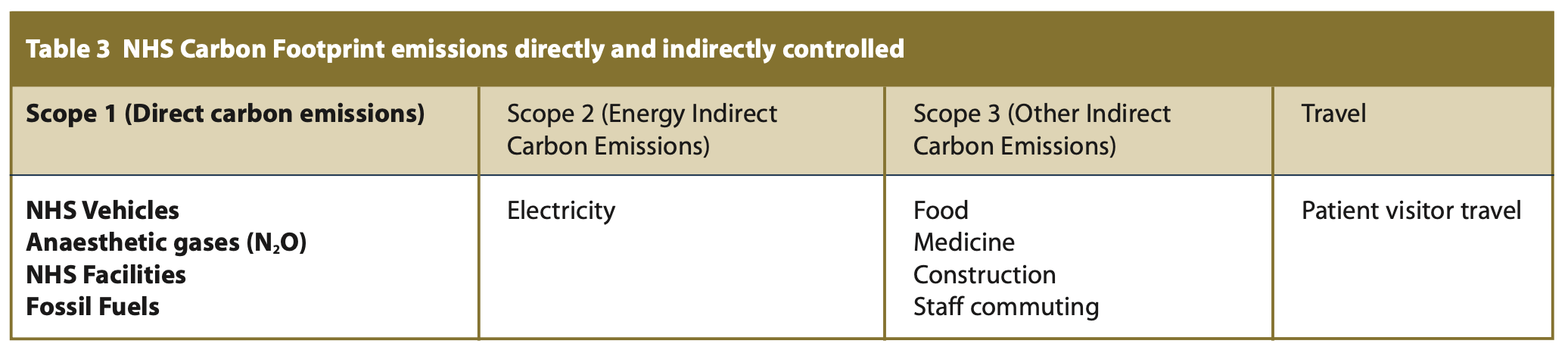
Improving clinicians’ awareness of the environmental impact of N2O, through improved education, increased access to information and stimulating new interest in environmental concerns, can allow for more sustainable N2O use. In recent years, there has been an increasing focus on sustainability and environmental emissions leading to wider discussions and an effort to improve environmental awareness and introduce waste mitigation strategies. In 2021, the Nitrous Oxide Mitigation Project was launched to recognise the declining use of N2O in routine anaesthetic practice and its significant environmental impact.18 The NHS' ‘Delivering a net zero NHS’ report was set out to combat the large NHS carbon footprint to directly control the emissions produced to net zero by 2040, and influence the emissions indirectly produced to net zero by 2045 (see Table 3). Scope 1 emissions are those from activities owned or controlled by organisations; examples of Scope 1 emissions include the emissions produced when N2O is used during IHS.
Nitrous oxide environmental and occupational exposure
To ensure the safe handling of N2O, measures aimed at preventing occupational exposures and environmental leaks must be implemented. The health and environmental impact of N2O is linked to its transportation, filling and general handling.19 The National Nitrous Oxide Project launched in January 2021 reported an annual system loss of 13,770,000L of N2O from piped manifold systems, representing roughly 95% of the total N2O procured.20 N2O that leaks into the environment can cause iatrogenic effects to clinicians, including dizziness, headaches and nausea, as well as waste into the atmosphere.
Mitigating against N2O waste involves using portable N2O cylinders, avoiding wasteful clinical practices, ensuring proper equipment, effective stock management and secure storage.18
Cylinders should be upright with secure valve caps, distinguishing between N2O (blue) and O2 (white), stored securely and accurately labelled indicating whether the cylinder is full or in use.19 When used excess N2O is removed by scavenging units set at 45 litres/minute to the outside environment to prevent unwanted iatrogenic effects. To further reduce the environmental impact of N2O, the dental community could consider carbon offsetting initiatives, such as investing in renewable energy or reforestation projects.
Administration
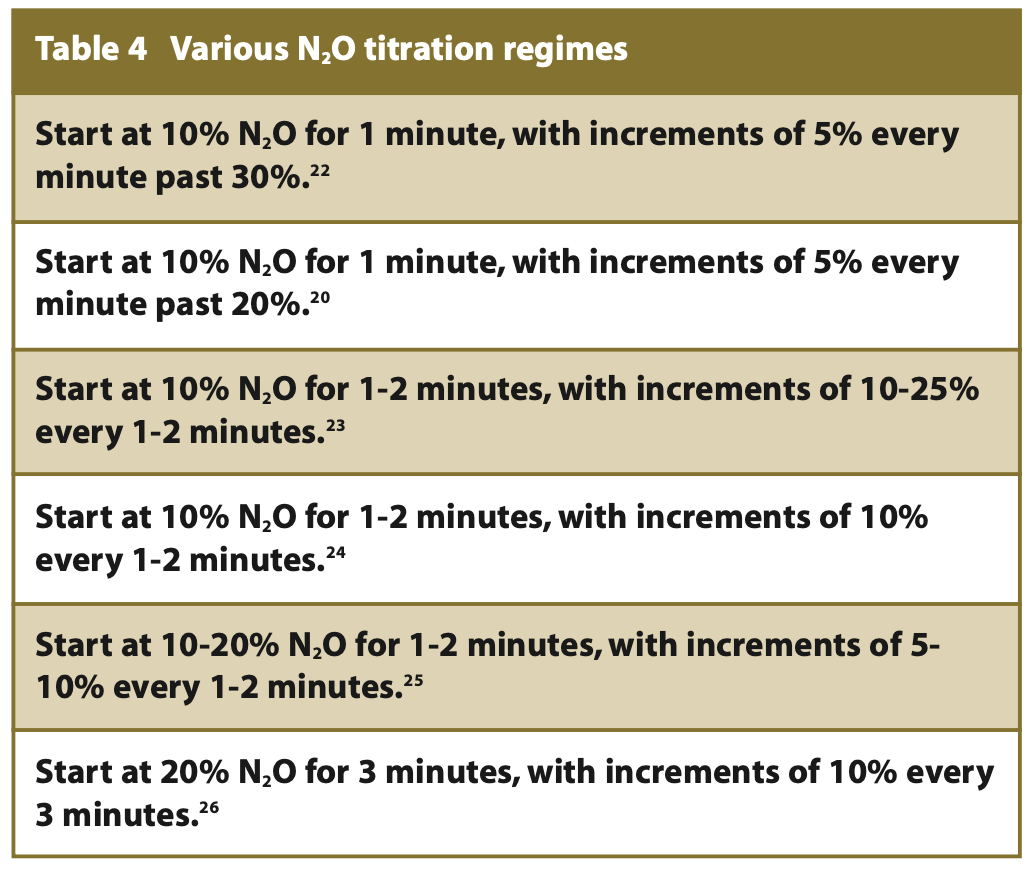
During the administration of N2O, factors such as the length of time, flow rate and the percentage of maximum N2O are required to calculate CO2e, thereby influencing carbon emissions per patient session. While time recorded is vital for CO2e calculations, it is not a standard practice to document to ensure safe conscious sedation.2 When establishing a flow rate of 5-6L/min is required to align with the breathing rate of most patients.21 During delivery, N2O should be titrated to prevent oversedation and unwanted side effects, but there are variations across the literature as to the correct titration regime (see Table 4).
When inhaled into the lungs, the distribution of inspired N2O throughout the body is influenced by gas tension and solubility. Gases of low solubility will reach tension and equilibrate rapidly in the bloodstream; it is the tension that provides the driving force of inhaled molecules to reach the brain.27 With low solubility, the blood concentration of N2O reaches equilibrium with alveolar concentration, thereby rapidly transported through the bloodstream to reach the brain inducing sedative effects. Becker and Rosenberg observed the kinetics of N2O and its onset of effect.27 Extrapolated data shows time against inspired N2O gas tension as a percentage shown in Table 5. The data highlights the progression of N2O equilibration, indicating after four minutes the equilibration within the alveoli plateaus. This data suggests longer lengths of time are needed to ensure sufficient N2O achieves equilibrium and is transported to the brain.
Local trends of N2O use
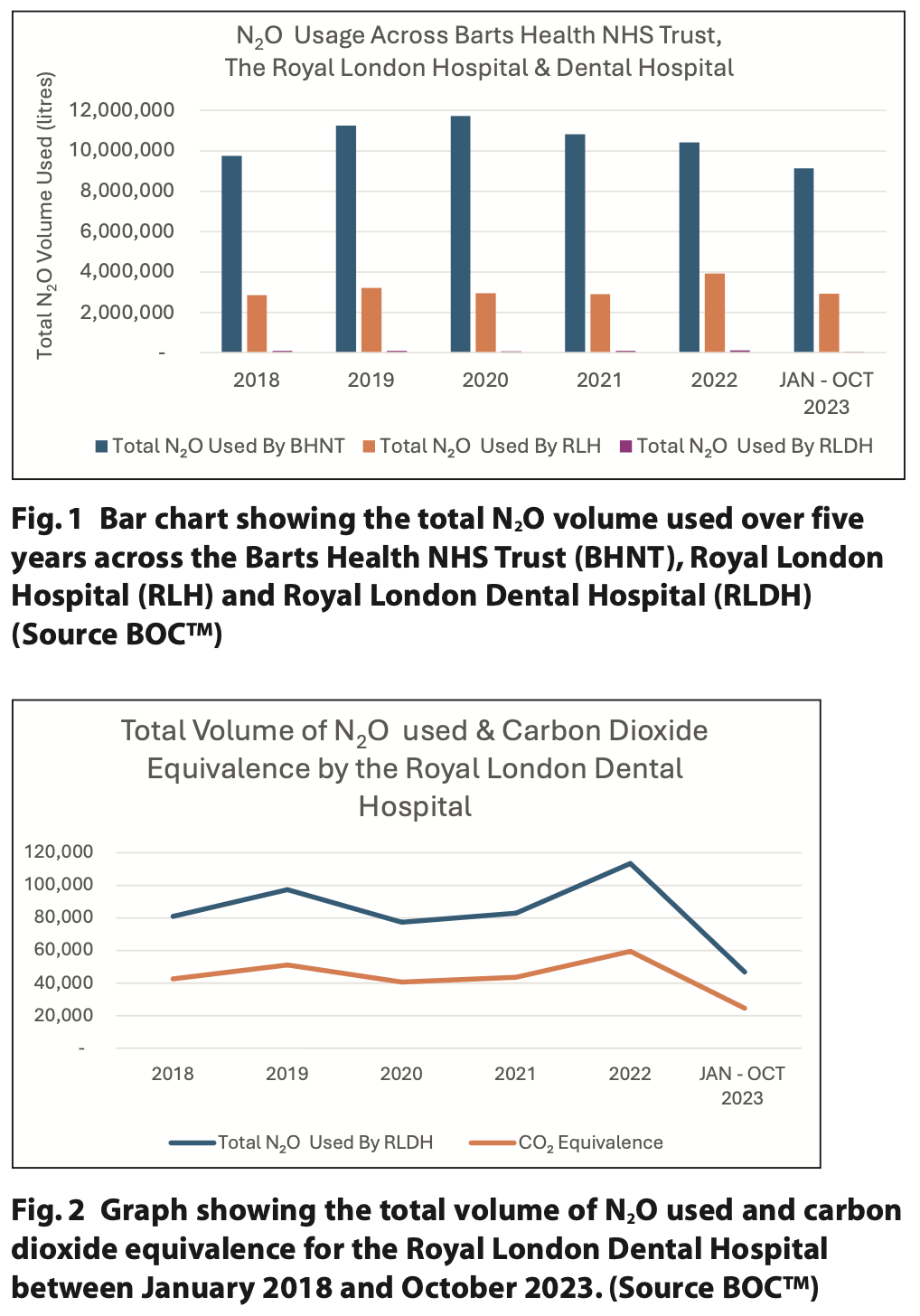
Over the last five years, data from BOC™ has shown that N2O usage at Barts Health NHS Trust (BHNT) has remained high, with the volume of N2O used by the RLDH presenting as a minute proportion of the total N2O used (see Figure 1). To provide context, the RLDH utilised 114,400 L of N2O in 2022, equivalent to driving 175,626 miles or circumnavigating the earth seven times.28 In comparison, the entire BHNT consumed 10,427,430 L in 2022, equating to driving 16,149,274 miles or encircling the earth 648.5 times. However, during the past five years there has been an overall steady decline in N2O volume used and CO2e at the RLDH (see Figure 2). This may be due to the shift in patient care pathways from secondary care to local provision in primary care, reducing the carbon footprint of associated travel to secondary care hubs.
Aims and objectives
N2O is a suitable and safer alternative to less resource-intensive and carbon emission-producing procedures such as GA. Demonstrating justified, successful and sustainable use of N2O is crucial for its continued use in dental conscious sedation. The primary aim of this quality improvement project (QIP) was to quantitatively record and compute CO2e per patient treatment and improve time recording of N2O usage to enable accurate carbon emission calculations. Treatment outcomes were assessed and mitigations for N2O will assess justification and success. The secondary aim was to qualitatively assess how clinicians were using N2O during procedures, assess if N2O cylinders are stored appropriately at the RLDH, and get feedback from clinicians on their views of N2O use.
Driver diagram
A driver diagram was used to help plan this QIP and future QIP / audits, providing theories about what changes will likely lead to our desired aim of providing environmentally sustainable IHS using N2O (see Figure 3).
Model of improvement
This project hopes to improve the time recording of N2O usage to enable accurate carbon emission calculations and raise awareness of the environmental impact of N2O amongst clinicians. The project seeks to highlight whether N2O use is justified and successful for IHS. The identified improvements include justified and successful treatment, recorded time of N2O usage, and valid extrapolation of CO2e. The anticipated outcome is that clinicians will adhere to ‘as low as reasonably possible’ (ALARP) principles when using N2O, ensure time is recorded for future CO2e calculations, and ensure IHS is the first line of treatment over more resource-intensive procedures such as GA.
Material and methods
This QIP was approved by the Clinical Effectiveness Team at The Royal London Hospital.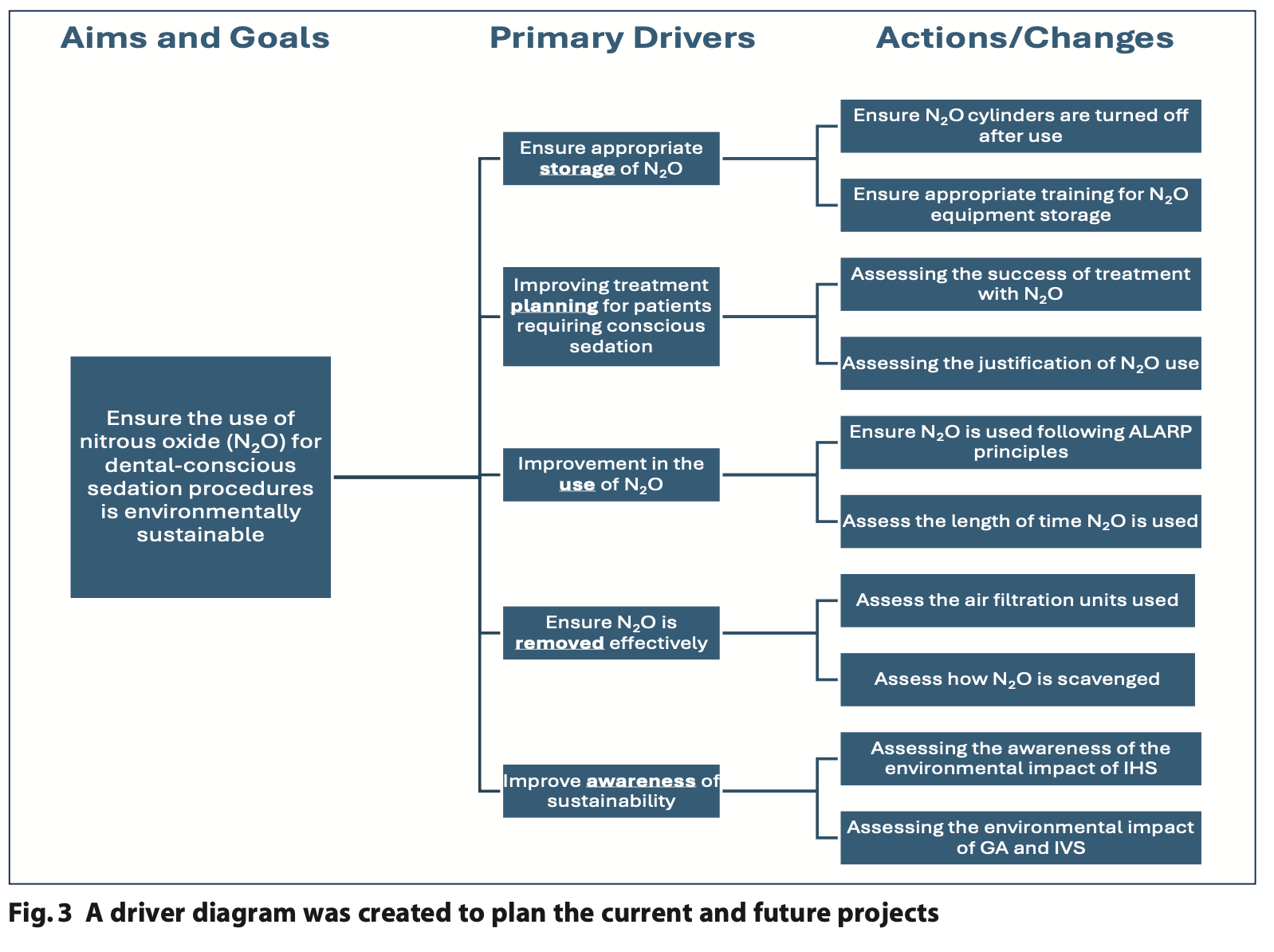 Sample
Sample
Preliminary retrospective data collection spanned three months across the Special Care (SC) and Paediatric departments; after implementing procedural changes emphasising N2O usage time, a subsequent one-month period was used to gather data prospectively to assess change and improvement. During the one month, spot checks of N2O cylinders and observations of clinicians using N2O were carried out across both departments. Feedback was then received from clinicians when results were discussed at a cross-department meeting.
Data collection
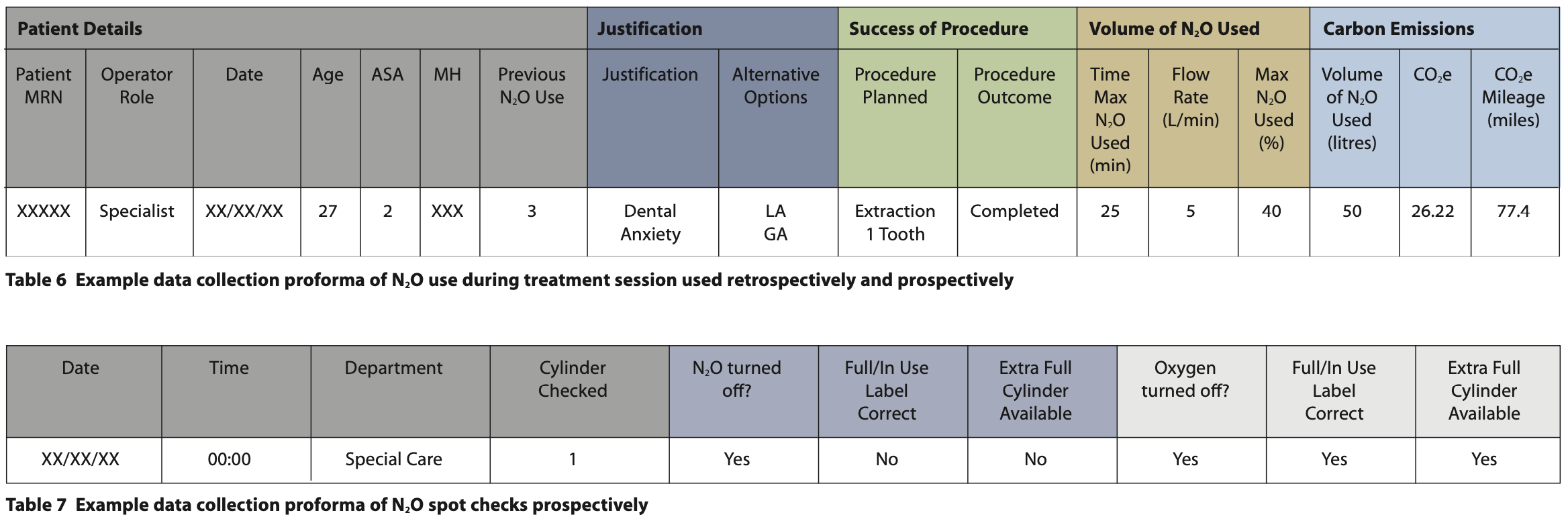
To comply with the General Data Protection Regulation (GDPR 2018), data were collected via the Trust’s computer system using the hospital database (Cerner Millennium). A data collection proforma was designed and validated (see Table 6). Collected data encompassed patient demographics (age, medical history and American Society of Anaesthesiologists Physical Status score,29 previous N2O use), treatment justification, alternatives, treatment outcomes, and carbon footprint calculation (N2O: volume, time of maximum usage, flow rate), the volume of N2O used, the CO2e and CO2e mileage were also recorded. The volume of N2O was calculated by multiplying the percentage of maximum N2O by the flow rate and time of maximum N2O used. CO2e is then calculated by multiplying this figure by 0.5244, which is then divided by 0.3386 to gain the CO2e mileage (see Table 2).
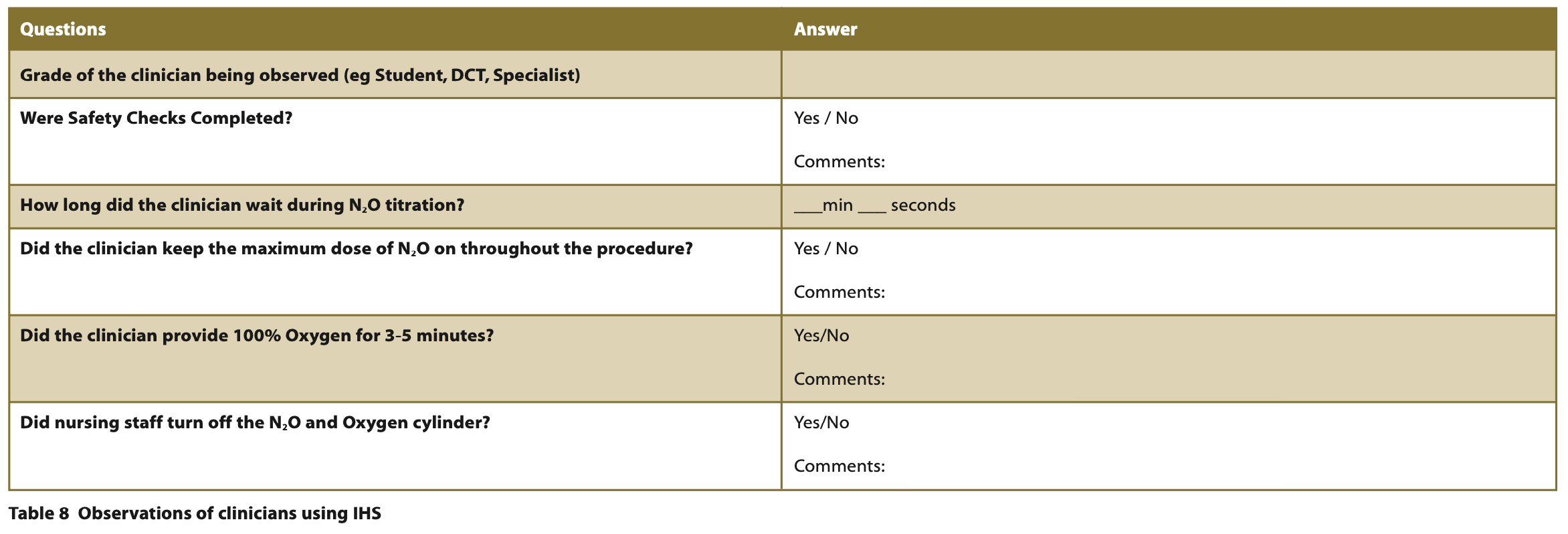
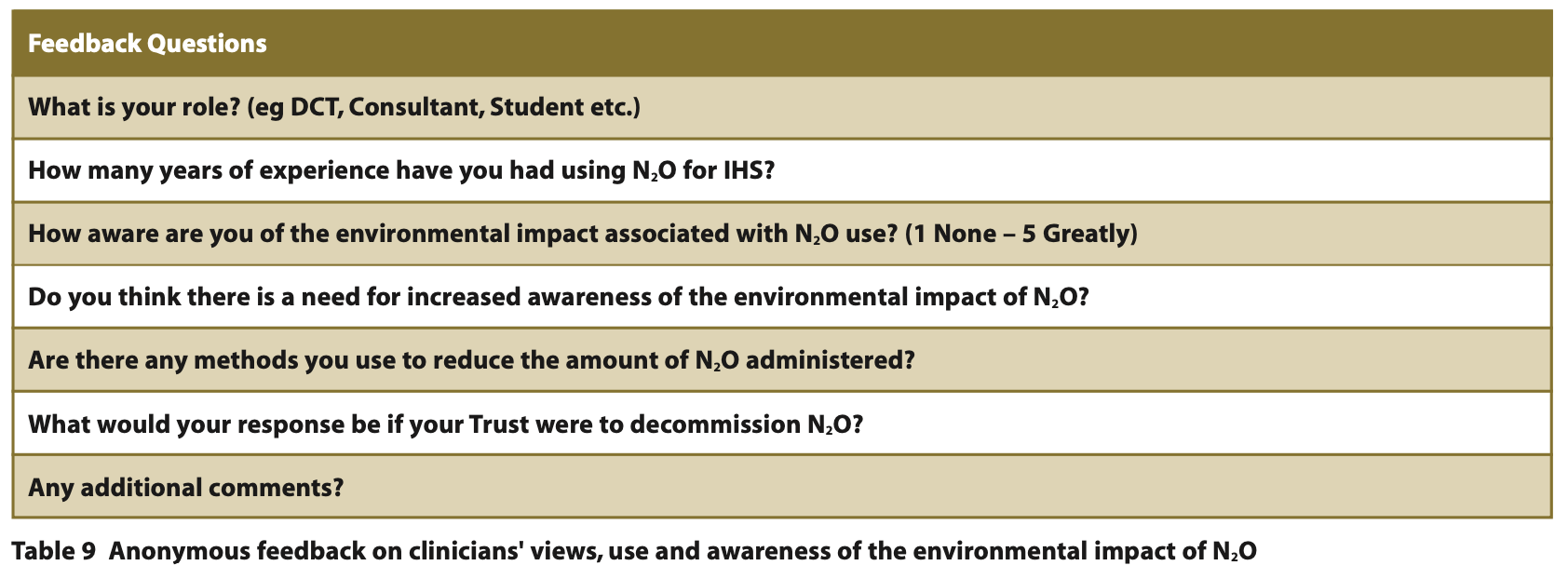
Spot checks of N2O and O2 were completed across the SC and Paediatric department, a data collection proforma was designed and validated (see Table 7). Spot observations took place across both departments, the form of which can be seen in Table 8. Feedback was asked of clinicians during a cross-department meeting, with an online questionnaire prepared using a Google form and distributed via a QR code allowing clinicians to provide feedback anonymously (see Table 9).
Data analysis
Data was stored and sorted on a secure online hospital hard drive and then analysed using a Microsoft Excel spreadsheet and Microsoft Word program.
Results
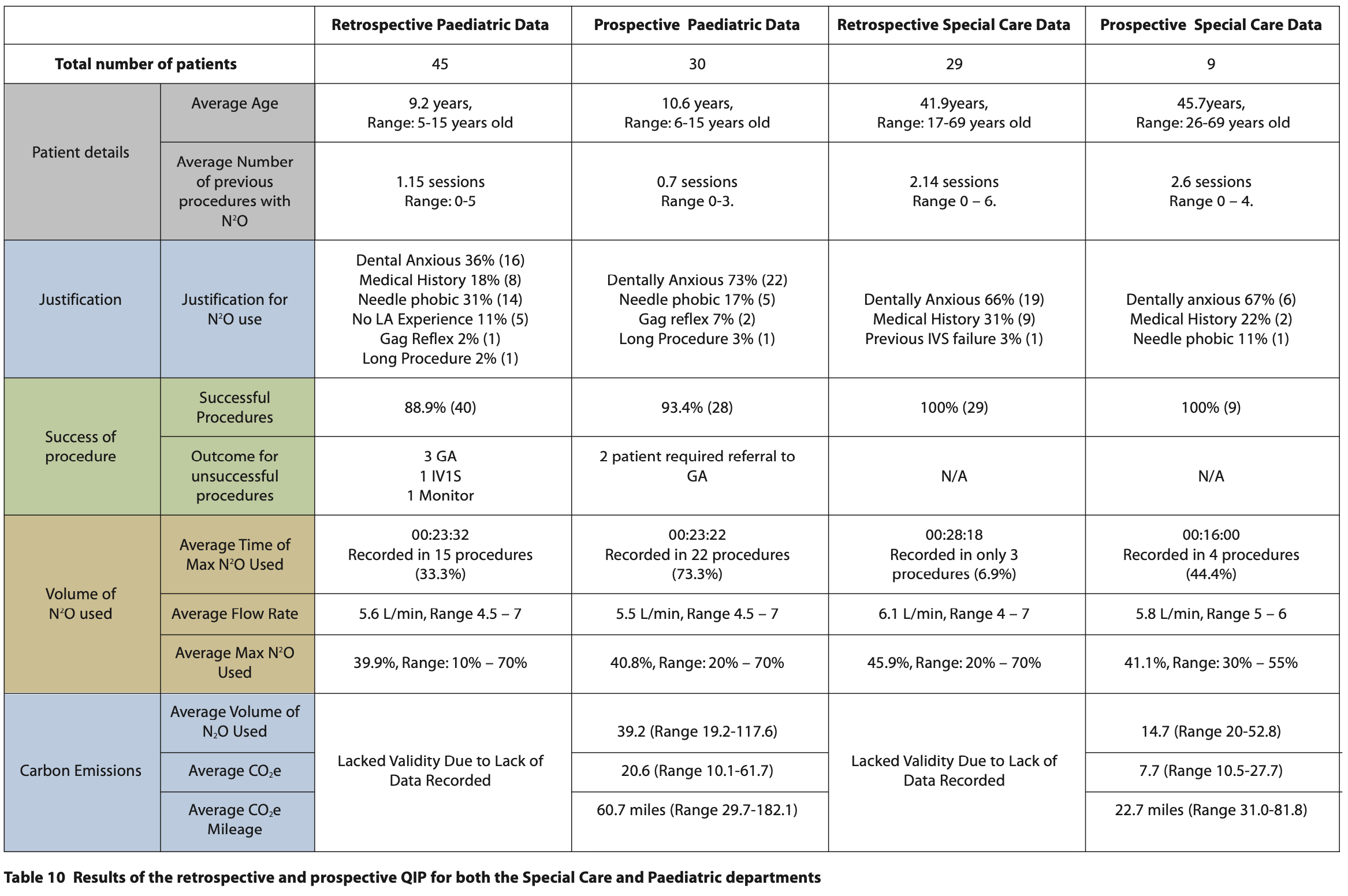
Data were collected retrospectively over three months (1 May to 31 July), and prospectively over one month (1 January to 31 January 2024), the results of which can be viewed in Table 10.
Patient Demographic
Retrospectively, the average age of patients in the paediatric department was 9.2 years, ranging between five and 15 years old. The average age of patients in the SC department was 41.9 years, ranging between 17 and 69 years old. Prospectively, the average age of patients in the paediatric department was 10.6 years, ranging between six and 15 years old. The average age of patients in the SC department was 45.7 years, ranging between 26 and 69 years old.
Justification
Data analysis confirmed consistent justification for the use of IHS using N2O retrospectively and prospectively in the paediatric department and SC department. Reasons for N2O use included dental anxiety, needle phobia, medical history, gag reflex, no LA experience, long procedure and previous IV failure.
Success
A high number of treatments were successful; retrospectively the paediatric department saw an 88.9% (n = 40) and SC 100% ( n= 29) success rate; prospectively the paediatric department saw a 93.4% (n = 28) and SC 100% (n = 9) success rate. Procedures that were not successful required either referral for GA, treatment under IVS or monitoring.
Time of N2O recording
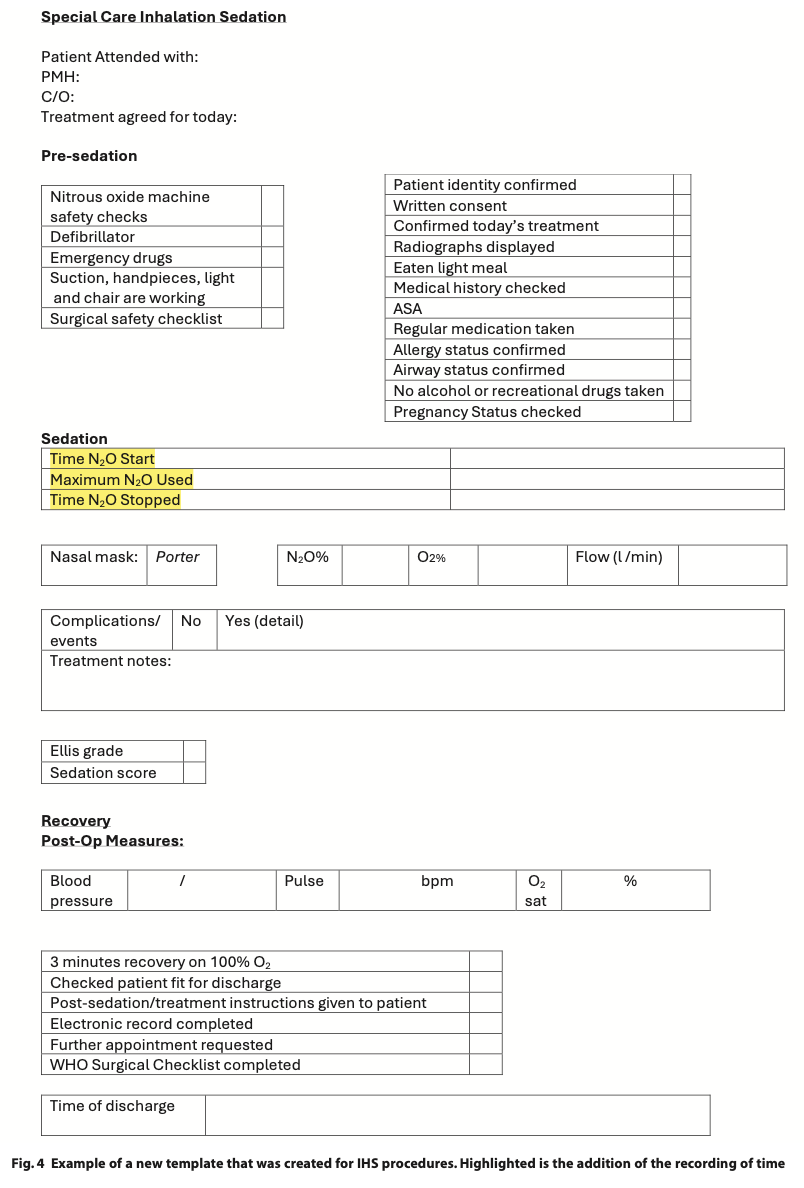
Retrospective data found a deficiency in recording N2O usage time, observed in only 33.3% (n = 15) of paediatric and 6.9% (n = 3) of SC treatment reducing the accuracy of carbon emission calculations and affecting their validity. After the implementation of a new IHS proforma, prospective data revealed 73.3% (n = 22) of paediatrics and 44.4% (n = 4) of SC treatments having time recorded.
Carbon emissions
Due to the lack of time recorded, the volume of N2O use, CO2e and CO2e mileage could not be recorded retrospectively in both departments. Prospective data showed in the paediatric department, the average volume of N2O used was 39.2 L, the average CO2e 20.6 and CO2e mileage of 60.7 miles. In the SC department, the average volume of N2O used was 14.7 L, the average CO2e 7.7 and CO2e mileage of 22.7 miles.
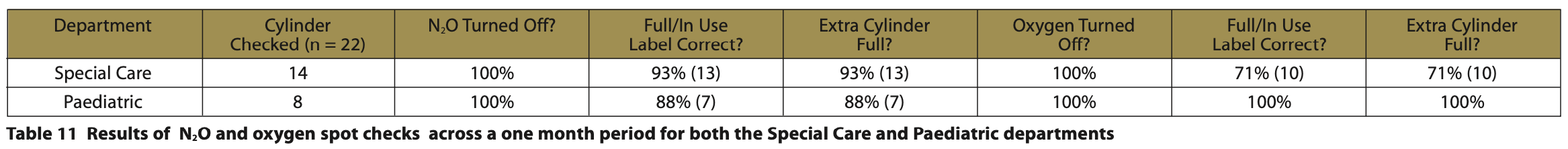
N2O storage
Over the one-month period (1 to 31 January 2024), a total of 22 cylinders were spot checked, 14 from the SC and 8 from the Paediatric department, the results of which can be viewed in Table 11. 100% of the N2O and 100% of the O2 cylinders were turned off across both departments. However, it was noted two N2O cylinders and four O2 cylinders with full / in use labels were missing or incorrectly labelled, and that these extra cylinders were not full on the portable N2O units.
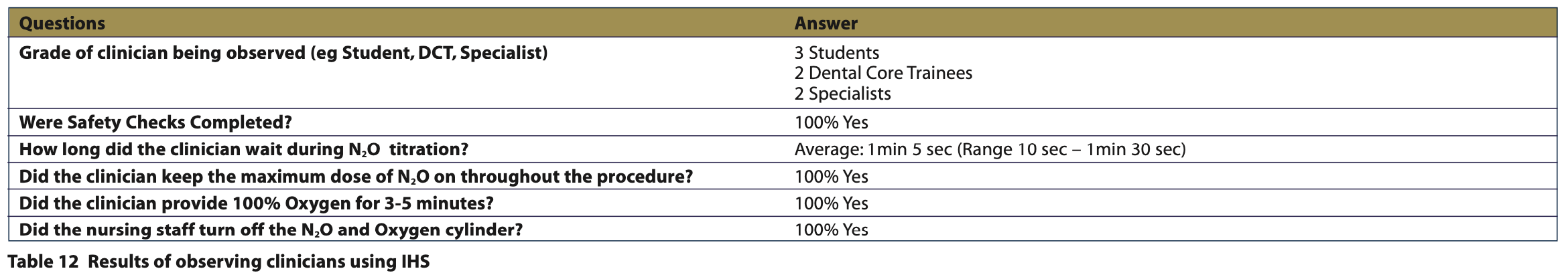
Observations of clinicians
Over the one-month period (1 to 31 January 2024), a total of seven clinicians were observed between each department the results of which can be seen in Table 12. All pre-operative and post-operative safety checks were completed, during treatment on average the majority of clinicians titrated N2O for 1 min 5 sec and all provided 3 to 5 minutes of O2 to prevent desaturation. All clinicians observed kept the maximum amount of N2O throughout the procedure.
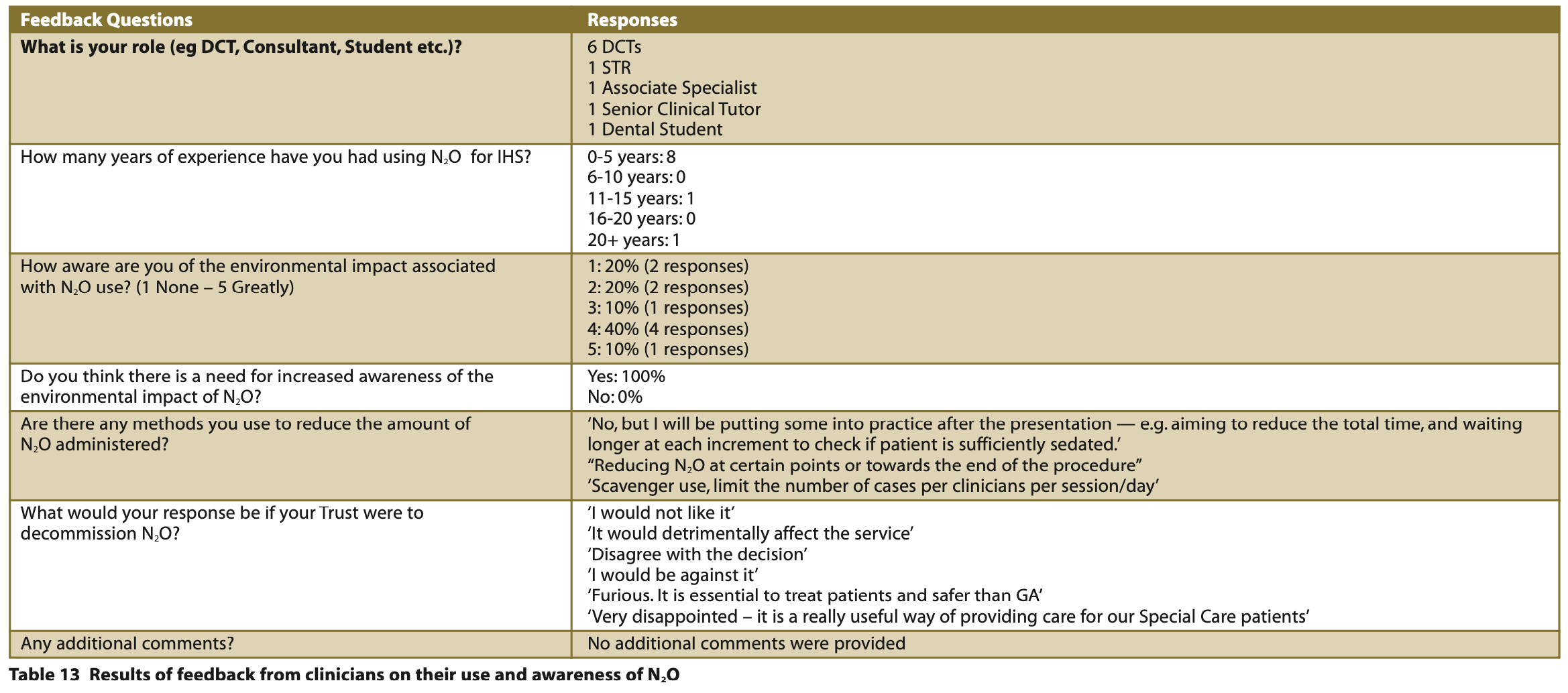
Feedback from clinicians
During a cross-department meeting, feedback was received from a total of ten clinicians the result of which can be viewed in Table 13. The survey captured a wide range of clinicians from trainees to consultants, with the majority having only zero to five years’ N2O experience. A spectrum of understanding was noted amongst clinicians, but unanimously agreed on the need for increased awareness regarding the environmental impact. In responses to a hypothetical scenario where BHNT were to decommission N2O, strong opposition was expressed; clinicians voiced disagreement and disappointment, the potential detriment and indispensability of N2O to patient care, and one clinician considered it safer than GA.
Discussion
The findings of this QIP present valuable insight into the use of N2O for IHS in a dental setting. The results indicate consistent justification and high treatment success rates when using N2O, with significant differences observed between the retrospective and prospective data. The QIP confirms a high success rate for treatment, this outcome underscores the effectiveness of N2O across both paediatric and SC departments.
Significant findings in the retrospective data found deficiencies and time recording of N2O usage, impacting carbon emission calculations which ultimately lacked validity. This limitation hindered the comprehensive understanding of the environmental impact associated with each patient session, hence the need for improvement. The findings of the retrospective data were presented at a cross-department meeting, with a new proforma provided to the clinicians to improve the recording of time which can be seen in Figure 4. Encouragingly, the prospective data showed a 543.5% increase and a 120.1% increase in time recorded in both the SC and Paediatric departments respectively. This then enabled valid carbon emission calculations to be evaluated.
From prospective data, the Paediatric department utilises a higher volume of N2O compared to the SC department. A plausible hypothesis is this increase may be linked to a larger and younger population of patients, for whom IHS is the sole option, in contrast to the SC department, where alternative options such as IVS are aligned with the specific needs of patients treated.
Concerning the storage of N2O and O2 cylinders, although the sample size assessed was small, it is reassuring to observe that all cylinders are being properly turned off when stored, reducing occupational and environmental exposure. However, discrepancies were identified including missing or incorrectly labelled full / in use labels with a full N2O or O2 cylinder not present on the portable system. This safety concern was raised at a cross- department meeting and brought to the attention of the Senior Dental Nurse responsible for the N2O units, who subsequently purchased new recyclable labels.
During observations, it was noted that safety protocols were followed, and it was encouraging to see that staff members store N2O appropriately. It was noted, however, that there was a range of titration regimes reflected in the literature (Table 4). Methods to reduce N2O administration and follow ALARP principles were communicated at a cross-department meeting. Suggestions such as understanding the patient’s anxiety and phobia, as well as determining the specific stage during treatment when maximum N2O is essential, can lead to a reduction in the overall quantity of required N2O. An example was given of a patient with needle phobia, who may require a higher concentration of N2O during local anaesthetic administration but could be provided with a lower concentration for the remainder of treatment. It is the author’s opinion that extending the duration beyond one minute for each titration step is recommended, as evidenced in the literature.27 Regimes such as providing 20% of N2O for three minutes and increments of 10% every three minutes may provide more time for patients to feel sedated at lower N2O doses.27 This, coupled with non-pharmacological management strategies, such as hypnosis, virtual reality headsets, lighting and voice control can mitigate the need for higher concentrations of N2O. The author appreciates that each clinical scenario and environment is different and that the observations carried out were limited to a small number of clinicians, nevertheless, these recommendations are justified in ensuring sustainable N2O practice.
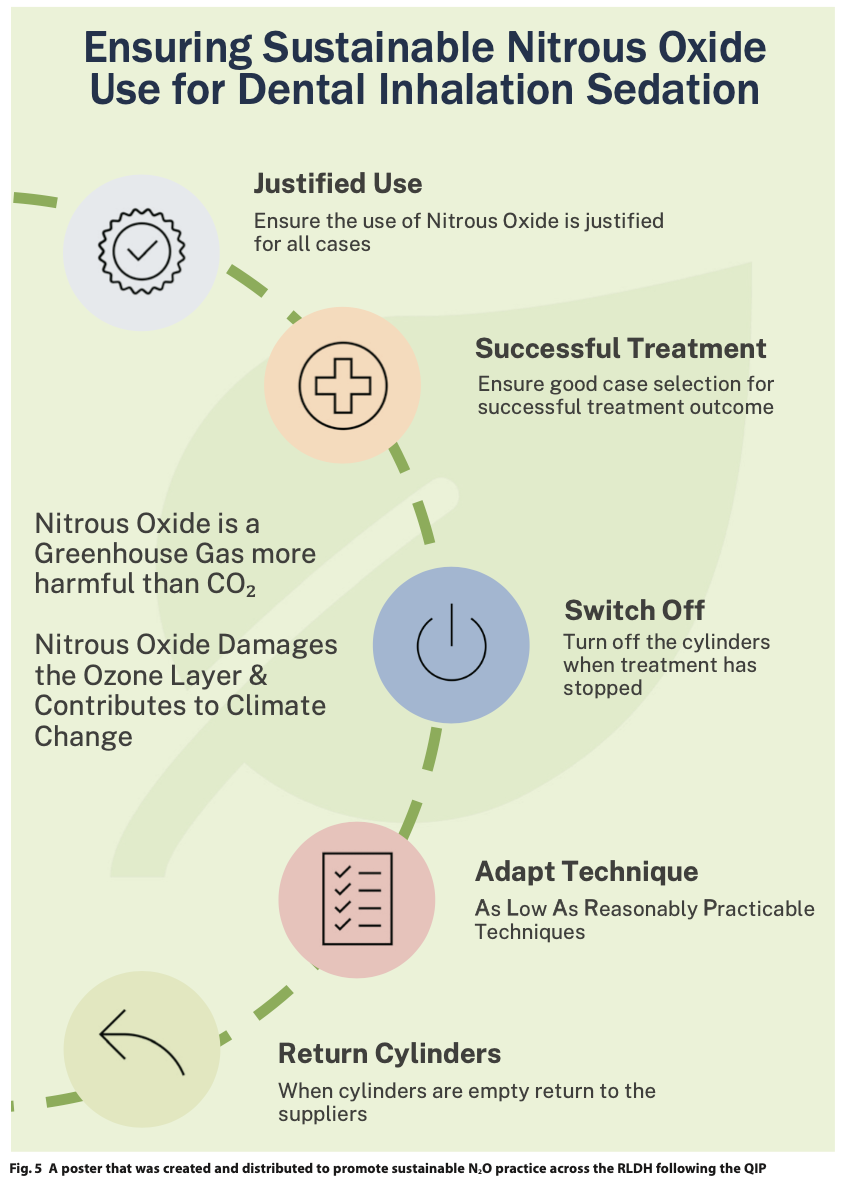
The consensus amongst clinicians highlighted the need for increased awareness of the environmental impact of N2O, regardless of the mixed awareness levels amongst the small sample size. It was encouraging to see clinicians employing strategies to reduce N2O administration, and their strong opposition to the decommissioning of N2O, with emphasis on its crucial role in patient care. The additional comments reveal a depth of sentiment and underscore the importance of considering clinicians’ perspectives in any future decisions related to N2O usage. Following the QIP, a poster was designed and distributed across the RLDH to educate clinicians and undergraduate students about promoting sustainable N2O use for dental IHS, which can be used as a tool for optimising N2O use in other settings (see Figure 5).
Conclusion
This QIP provides valuable insight into the use of N2O for IHS in both the SC and Paediatric departments in a dental setting. The results highlight consistent justification and high treatment success rate, affirming the effectiveness of IHS treatment when using N2O. Retrospective data showed deficiencies in time recording, impacting carbon emission calculations. After improvements were communicated, prospective data showed significant improvements in recorded time, enabling valid calculations, with the Paediatric surpassing the SC department in its use of N2O attributed to a larger, younger patient population. Environmental leakages were mitigated and other safety discrepancies were addressed promptly. The observations highlighted adherence to safety but identified variations in titration regimes. Recommendations and emphasis on sustainable N2O practice were communicated as well as the need for increased environmental awareness. The findings of this QIP underscore N2O's crucial role in treating patients through IHS, urging consideration of clinicians’ perspectives in future decisions regarding decommissioning.
Conflict of interest
The author declares no conflicts of interest.
References
1. Academy of Medical Royal Colleges. Safe Sedation Practice for Healthcare Procedures; An update. 2021. Online information available at: https://www.aomrc.org.uk/wp-content/uploads/2021/02/Safe_sedation_practice_for_healthcare_procedures_update_0521.pdf (accessed September 2024).
2. Royal College of Surgeons of England. 2020. Standards for Conscious Sedation in the Provision of Dental Care (V1.1): Report of the Intercollegiate Advisory Committee for Sedation in Dentistry (IACSD). Online information available at https://www.saad.org.uk/IACSD%202020.pdf (accessed September 2024).
3. National Institute for Health and Care Excellence. 2010. Sedation in under 19s: using sedation for diagnostic and therapeutic procedures (CG112). Online information available at: https://www.nice.org.uk/guidance/cg112/resources/sedation-in-under-19s-using-sedation-for-diagnostic-and-therapeutic-procedures-pdf-35109386077381 (accessed September 2024).
4. Knuf K, Maani C V. Nitrous Oxide. In: StatPearls. Treasure Island (FL): StatPearls Publishing. 2024. Online information available at: https://www.ncbi.nlm.nih.gov/books/NBK532922/ (accessed September 2024).
5. Li X, Liu Y, Li C, Wang J. Sedative and adverse effect comparison between oral midazolam and nitrous oxide inhalation in tooth extraction: a meta-analysis. BMC Oral Health. 2023; 23, 307.
6. Rossit M, Gil-Manich V, Ribera-Uribe J M. Success rate of nitrous oxide-oxygen procedural sedation in dental patients: systematic review and meta-analysis. J Dent Anesth Pain Med. 2021;21(6):527-545.
7. Vanhee T, Lachiri F, Van Den Steen E, Bottenberg P, Vanden Abbeele A. Child behaviour during dental care under nitrous oxide sedation: a cohort study using two different gas distribution systems. Eur Arch Paediatr Dent. 2021; 22, 409-415.
8. Wilson K. Overview of paediatric dental sedation: 2. nitrous oxide/oxygen inhalation sedation. Dental Update. 2013; 40:10, 707-709.
9. Greener NHS. Delivering a 'Net Zero' NHS. 2020. Online information available at: https://www.england.nhs.uk/greenernhs/a-net-zero-nhs/ (accessed September 2024).
10. Forster P V, Ramaswamy P, Artaxo T, et al. Changes in Atmospheric Constituents and in Radiative Forcing. In: Climate Change 2007: The Physical Science Basis. Contribution of Working Group I to the Fourth Assessment Report of the Intergovernmental Panel on Climate Change [Solomon, S., D. Qin, M. Manning, Z. Chen, M. Marquis, et al. (eds.)]. Cambridge University Press, Cambridge, United Kingdom and New York, NY, USA. Online information available at: https://www.ipcc.ch/site/assets/uploads/2018/02/ar4-wg1-chapter2-1.pdf (Accessed September 2024).
11. Prather M J, Hsu J, DeLuca N. et al. Measuring and modeling the lifetime of nitrous oxide including its variability. J. Geophys. Res. D. 2015; 120, 5693–5705.
12. Stocker T, Qin D, Plattner G. et al. in Climate Change 2013: The Physical Science Basis (eds Stocker, T. F. et al.) Ch. 6 (IPCC, Cambridge Univ. Press, 2013).
13. Public Health England. Carbon modelling within dentistry - Towards a sustainable future. 2018. Online information available at: https://www.gov.uk/government/publications/carbon-modelling-within-dentistry-towards-a-sustainable-future (accessed September 2024).
14. Chakera A. The Nitrous Oxide Project: #nixthenitrous. Online information available at: https://www.ed.ac.uk/medicine-vet-medicine/postgraduate/postgraduate-blog/the-nitrous-oxide-project-nixthenitrous (accessed September 2024).
15. Brander M. Greenhouse Gases, CO2, CO2e, and Carbon: What Do All These Terms Mean? Ectometrica. 2023. Online information available at: https://ecometrica.com/assets/GHGs-CO2-CO2e-and-Carbon-What-Do-These-Mean-v2.1.pdf (accessed September 2024).
16. ZeroCO2. What is CO2 equivalent (CO2e) and how is it calculated)? 2022. Online information available at: https://zeroco2.eco/en/magazine/environment/co2-equivalent/ (accessed September 2024).
17. Chaekera A. Evidence-Based Policy Report: Reducing Environmental Emissions attributed to Piped Nitrous Oxide Products within NHS Hospitals. Online information available at: https://www.sehd.scot.nhs.uk/publications/piped-nitrous-oxide-products.pdf (accessed September 2024).
18. Chakera A, Fennel-Wells A, Allen C. Piped Nitrous Oxide Waste Reduction Strategy. Nitrous Waste Methodology. 2021. Online information available at: https://anaesthetists.org/Portals/0/PDFs/Environment/Nitrous%20waste%20methodology.pdf?ver=2021-04-26-115439-240 (accessed September 2024).
19. EIGA Doc 176. Safe Practice for Storage and Handling of Nitrous Oxide. Online information available at: https://www.eiga.eu/uploads/documents/DOC176.pdf (accessed September 2023).
20. Association of Anaesthetists. The nitrous oxide project. 2021. https://anaesthetists.org/Home/Resources-publications/Environment/Nitrous-oxide-project Online information available at: (accessed September 2024).
21. Associate of Anaesthetists. Guide to green anaesthesia. 2024. Online information available at: https://anaesthetists.org/Home/Resources-publications/Environment/Guide-to-green-anaesthesia (accessed September 2024).
22. Wilson K. Overview of paediatric dental sedation: 2. nitrous oxide/oxygen inhalation sedation. Dental Update. 2013; 40:10, 707-709.
23. Dental Economics. Nitrous Oxide. A Refresher Course. Online information available at: https://www.dentaleconomics.com/science-tech/article/16384940/nitrous-oxide-a-refresher-course (accessed September 2024).
24. American Academy of Pediatric Dentistry. Use of nitrous oxide for pediatric dental patients. The Reference Manual of Pediatric Dentistry. Chicago, Ill.: American Academy of Pediatric Dentistry. 2023; 393-400.
25. Aboytes D. Administration of Nitrous Oxide Analgesia. Decisions in Dentistry. Online information available at: https://decisionsindentistry.com/article/administration-nitrous-oxide-analgesia/ (accessed September 2024).
26. Jayaraman J. Effective Nitrous Oxide/Oxygen Administration for Children. DentalCare. Online information available at: https://assets.ctfassets.net/u2qv1tdtdbbu/tPrM8VCUa0tnI0zBWnl35/bf4865e6e90cef098cf4774701438923/ce92_12-16-21.pdf (accessed September 2024).
27. Becker D E , Rosenberg M. Nitrous oxide and the inhalation anesthetics. Anesthesia progress. 2008; 55(4), 124–132.
28. Star Alliance. Round the World. Online information available at: https://roundtheworld.staralliance.com/staralliance/en/round-the-world (accessed September 2024).
29. ASA Physical Status Classification System. American Society of Anesthesiologists. 2020. Online information available at: https://www.asahq.org/standards-and-guidelines/asa-physical-status-classification-system (accessed September 2024).