Please click on the tables and figures to enlarge
Dentist-led conscious sedation with remimazolam in a frail older adult
K. Wyncoll*1 BDS MFDS RCSEd
L. Charles2 BDS MFDS RCPS (Glasgow)
X. Yeo3 BDS MSc Dental Implantology DipConSed MFDS RCPS(Glasgow) PgCert Dental Education CILT AKC
H. Hossenally4 BDS MFDS RCS MSCD RCSEd MSc CILT
S. Clough5 BChD MFGDP (UK) MFDS RCS (Eng) MJDF MSpec Care Dent MSc CILT
1DCT1 in Special Care Dentistry, Barts Health NHS Trust, Royal London Dental Hospital, Turner Street, London, E1 1FR
2DCT2 in Special Care Dentistry, Barts Health NHS Trust, Royal London Dental Hospital, Turner Street, London, E1 1FR
3Speciality Trainee Registrar in Special Care Dentistry, Barts Health NHS Trust, Royal London Dental Hospital, Turner Street, London, E1 1FR
4,5Consultant in Special Care Dentistry, Barts Health NHS Trust, Royal London Dental Hospital, Turner Street, London, E1 1FR
*Correspondence to: Dr Kate Wyncoll
Email: kate.wyncoll@nhs.net
Wyncoll K, Charles L, Yeo X, Hossenally H, Clough S. Dentist-led conscious sedation with remimazolam in a frail older adult. SAAD Dig. 2025: 41(I): 32-35
Abstract
Special care dentistry manages patients with multiple co-morbidities that present challenges for delivery of dental care. Treatment planning in this cohort requires a holistic and flexible approach. A 69-year-old male patient presented with multiple carious retained roots suspected to be causing pain. The patient was non-verbal and had a severe learning disability, dysphagia and frailty.
Initially, a general anaesthetic was planned to complete comprehensive dental care. However, by the day of the procedure, the patient’s frailty had deteriorated and he was not deemed fit for a general anaesthetic. To avoid a loss of theatre space and clinical activity, as well as to facilitate completion of the required dental treatment, the dental team worked with the anaesthetic team, adapting the treatment plan to perform intravenous sedation in theatre with the novel benzodiazepine remimazolam.
This case highlights the dynamic nature of treatment planning in frail multi-morbid patients where the clinical picture can change significantly between appointments. Frailty is becoming ever more pertinent with our ageing population. This case demonstrates the use of intravenous sedation with remimazolam as a potential solution in these cases.
Case Summary
Midazolam has been the drug of choice for intravenous conscious sedation in dentistry for many years, but it does have limitations. It may not be suitable for patients with dysphagia, or for older frail patients due to the potential for prolonged recovery and further complications.1 This case report describes an older, frail patient with dysphagia, who was treated with intravenous (IV) remimazolam in a theatre setting after being deemed high risk for a general anaesthetic. It demonstrates how this emerging drug is very beneficial in enabling the treatment of patients who are otherwise unsuitable for IV sedation with midazolam or general anaesthetic.
Patient details
Gender: Male
Age at start of treatment: 69
Pre-treatment asessment
History of presenting patient’s complaints
- Attended with his carers of seven years, who reported signs that he was in pain from his teeth, including hitting his face and rubbing staff members’ hands on his cheeks.
Relevant medical history
- Severe learning disability
- Dysphagia
- Osteoarthritis
- Stable schizophrenia
- Previous aspiration pneumonia 2023
- Wheelchair user for the last three years, mobility declining due to age-related arthritic changes.
Medication
- 2.5 mg Amlodipine
- 30 mg Lansoprazole
- 15 mg Olanzipine
- 250 mg Valproic acid
- 100 mg Docusate
- 5 mg Procyclidine
- 50 mg Sertraline
Dental history
- He was seen on a domiciliary basis by the community dental service
- Carers supported him with oral hygiene, using a ‘special shaped brush’ and fluoride toothpaste
- No history of sedation, but compliant with blood tests.
Social history
- Lived in residential care, in a bungalow
- Had a sister who was involved in his care, but she was unwell herself so was unable to be involved in any decisions. She was contacted and agreed what was in the best interest of the patient.
Clinical examination
- The patient could self-transfer from the wheelchair to the dental chair
- Limited examination carried out without mirror or probe due to lack of patient co-operation
- Multiple carious retained roots visualised
- Poor oral hygiene
- Generalised gingival inflammation
- Mental capacity assessment carried out and patient was deemed not to have capacity as he was unable to understand, weigh up, retain or communicate a decision.
General radiographic examination:
- Radiography was not possible due to patient movement. Any images would have been non-diagnostic.
Best interests meeting
- Attended by dental staff, patient’s carers and service delivery manager
- Risks and benefits of no treatment discussed, including risk of further decline in frailty making future treatment very difficult and risk of further pain and infection
- Treatment modalities discussed including IV sedation with midazolam or comprehensive treatment under general anaesthetic. At this point in time remimazolam was not approved for use in the Trust
- Agreed treatments were dental examination, radiographs and any necessary dental treatment under general anaesthetic. The pre-operative and post-operative periods were discussed including the potential for an overnight stay, the need for a soft diet, and involvement of the Speech and language team (SALT) team was planned.
Reassessment on day of surgery
- By the time of the surgery 11 months after initial assessment, the patient’s condition had deteriorated. A hoist was now required for transferring the patient
- The patient was frail with poor muscle tone, slow movements and drooling
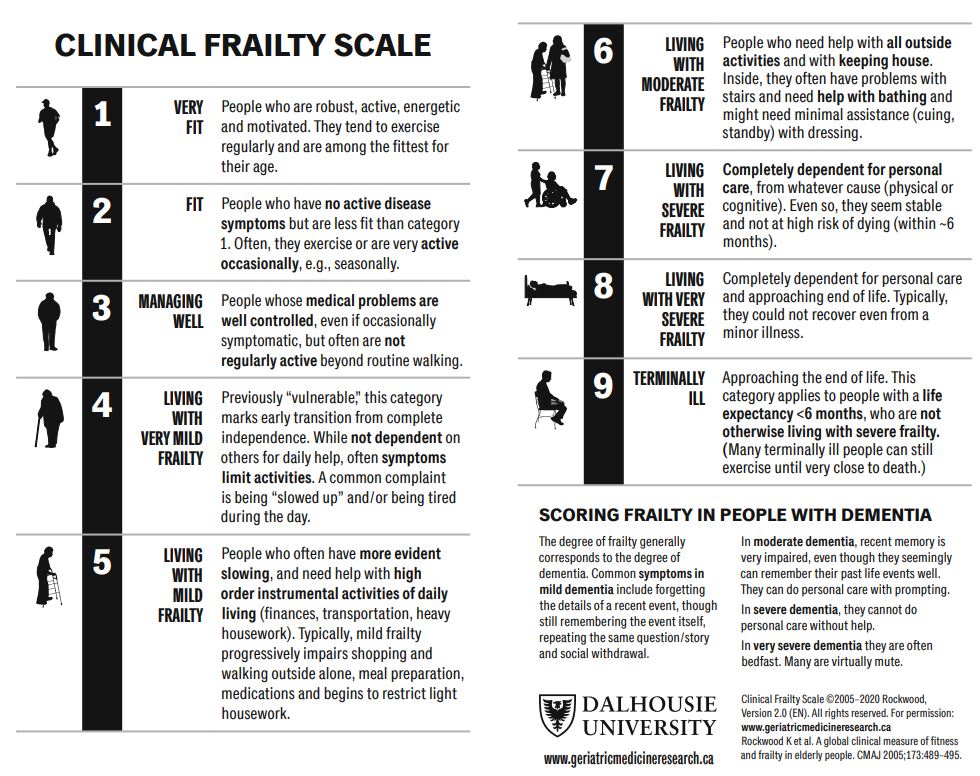
- The anaesthetist assigned a Rockwood frailty score2,3 of 7 (Fig. 1), and had concerns about the impact of the GA on a patient with this level of frailty
- The patient was able to be managed as a day case as he was accompanied by two carers and did not require admission as an in-patient for observation.
Revised treatment options:
- Treatment under general anaesthetic following a high-risk assessment. This would mean postponing the general anaesthetic to a future date
- Treatment with IV sedation using remimazolam. This drug was not available for use when the patient was initially assessed. The dental team had been using remimazolam regularly for IV sedation for the previous six months.
Diagnostic summary
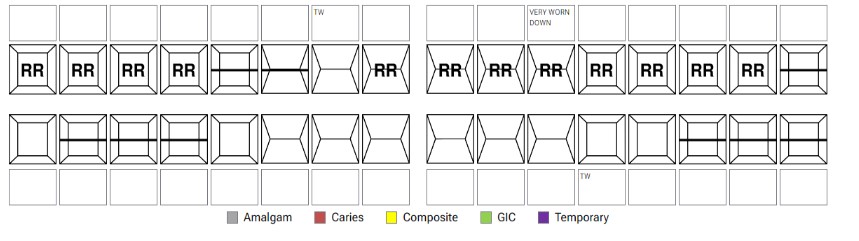
- Carious retained roots UR87651, UL1234567
- UR2 sharp
- Generalised gingivitis.
Aims and objectives of treatment
- Resolve pain related to the multiple retained roots
- Resolve pain related to the sharp UR2
- Prevent future pain and infection
- Stabilise dentition
- Treat the patient safely, avoiding risks associated with a high- risk general anaesthetic.
Fig.1 Rockwood frailty score. Source: Dalhousie University
Treatment plan
1. IV sedation with remimazolam to be carried out by the dental team with additional monitoring and support from the anaesthetic team for:
- Extraction of retained roots UR87651, UL1234567
- Smoothing of UR2
- Scaling to remove calculus on lower anterior teeth
2. Discharge to Community Dental Service for ongoing monitoring and prevention.
Treatment undertaken
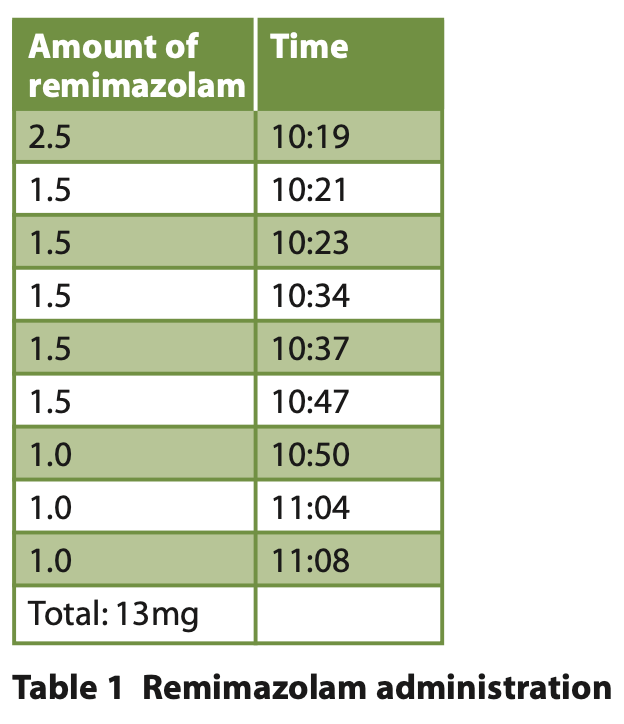
- IV access was gained using low level clinical holding. No oral premedication was required. A total of 13 mg remimazolam was given over 49 minutes. (See Table 1 for details of the top-ups given)
Fig. 2 Dental charting
- Local anaesthesia was achieved with 2 x cartridges 2.2ml 2% lidocaine, 1:80,000 adrenaline given as buccal and palatal infiltrations and 2 x cartridges 2.2 ml 4% articaine 1:100,000 adrenaline given as buccal and palatal infiltrations
- UR87651 and UL1234567 were extracted, and all sockets packed and sutured with Surgicel and vicryl rapide 3/0
- Low level clinical holding by one person was required to keep the patient’s hand still, to allow cannulation and to support the patient’s head during treatment
- Treated in Fowler’s position (Figure 3), with the upper body at about 60° to help maintain the airway. This was achieved in theatre by the dental team hoisting the patient onto a hospital bed and taking him to theatre, where the back of the bed was then raised to allow a 60° incline with then additional use of pillows.
Fig. 3 Fowler's position
- High volume aspiration was used throughout at close range to the surgical site in order to maintain a clear airway by an experienced dental nurse
- A dedicated dentist experienced in the administration of remimazolam was solely responsible for the sedation, while another dentist carried out the dental treatment
- Capnography was used by the anaesthetist to monitor the patient throughout. SpO2 was maintained at over 95%
- Radiographs were not taken due to the patient not being able to bite down on the holder and keep still. Imaging would not have changed management and therefore it was not in the patient's best interest to prolong the sedation time
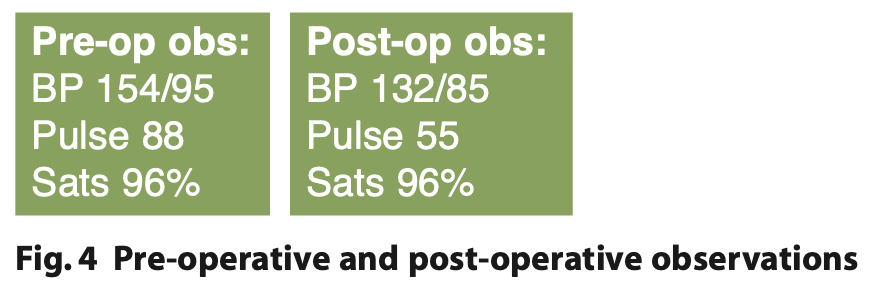
- The patient was discharged after a short recovery period of approximately 15 minutes in a designated recovery area with a satisfactory haemodynamic status compared to baseline (Figure 4).
Long term treatment and future considerations
The challenge in treating this patient was the changing clinical picture due to their progressing frailty. The patient may continue to deteriorate along the frailty scale, making future treatment more difficult. However, the availability of remimazolam provides an option for any future treatment required to be carried out in a safe manner without the need for a high-risk general anaesthetic. This also means that more conservative treatment could be carried out, maintaining non-carious teeth.
The patient can now be seen in community dental services for regular assessment and prevention.
Discussion and reflection about case presented
The patient’s best interests were the highest priority, with treatment under IV remimazolam enabling treatment to proceed on the day and allowing safe delivery of care. The theatre setting with additional monitoring and support from the anaesthetic team enhanced safety, allowing early detection and prompt management of any potential complications. Proceeding with treatment using remimazolam sedation utilised the theatre slot allocated to the patient, avoiding the waste of precious resources and time.
There was an anaesthetist present during this case, however, they did not become involved in the delivery of sedation as they had no experience in the technique or drug. As they were available and willing to assist, they aided the team with the clinical and mechanical monitoring of the patient, however, this could have been carried out by the sedationist and the case therefore could have been managed in primary care or a community clinic without anaesthetic support. Due to the short half-life of remimazolam and the need to constantly administer the drug, as well as the additional monitoring for this case, a separate trained sedationist would be necessary.
At the time of planning this case, the patient was not sent for an anaesthetist led pre-assessment as the dentist assessed the patient and he did not meet the criteria at this time. However, this is something that we do where indicated in high-risk cases to ensure appropriate planning of general anaesthetics for these patients.
Frailty is becoming an increasingly prominent aspect of treatment planning in dental care for elderly patients.4 Medical advancements mean patients are living longer with more comorbidities, including those with learning disabilities.5 It is important that the potential for decline in condition is considered at the early stages of treatment planning and discussed with family or carers. This includes acknowledging that treatment plans may evolve over time as the clinical picture changes. There must be reassessment at each appointment to ensure that plans previously made are still safe and remain in the patient’s best interests.
Safe and effective treatment in this case was possible due to the emerging drug remimazolam which was approved for use in dentistry by the Intercollegiate Advisory Committee for Sedation in Dentistry (IACSD) in January 2023.6 It has been regularly used in special care dentistry at Bart’s Health NHS Trust since March 2023. The benzodiazepine combines the properties of midazolam and remifentanil and has the same reversal agent as midazolam; flumazenil.7 There is little published data on its use in dentistry, but initial medical trials have demonstrated its ultra-short acting nature, with an onset of action of 1-3 minutes, a half-life of 7-8 minutes, and patients becoming fully alert 12-14 minutes after the last dose.8,9 This makes it ideal for frail patients and those with a higher dysphagia risk, as the time to recovery is much reduced compared to midazolam. Its organ-independent metabolism and elimination also makes it suitable for use in patients with hepatic or renal failure.7
Titration of remimazolam can be adjusted throughout the procedure based on observing the patient’s level of sedation and the stage of clinical procedure. More regular top-ups can be given for more invasive or unpleasant parts of the procedure, for example in this case, during the extractions to allow safer compliance. The short half-life enables finer control over the sedation window. This also means the sedation window can be extended with additional top-ups for as long as required without the risk of prolonging the recovery.
This case demonstrates the benefits of remimazolam in frail, older patients who benefit from the shorter recovery and are more sensitive to midazolam. The faster recovery means a complete return to their psychomotor functions, less disorientation and results in less risk of post-operative complications such as delirium and falls, reducing the burden on carers. It also avoids the risks of over-sedation and respiratory depression found with midazolam. Remimazolam expands treatment options for patients who were previously not suitable for IV sedation with midazolam, allowing treatment in a less restrictive and invasive way than a general anaesthetic. However, it remains very important to assess patients individually, taking into account their medical, dental and social histories.
Dosing guidelines from the manufacturer suggest an initial dose of 7 mg over 1 minute, waiting 2 minutes, then further top-ups of 2.5 mg as required to maintain sedation for adults under the age of 65.10 For those over 65, ASA III-IV or body weight under 50 kg, recommended initial dose is reduced to 2.5-5 mg, waiting two minutes, then further injections of 1.25-2.5 mg as required. However, further research is needed into this and specifically into its use in dental sedation.
The request for approval of remimazolam at Barts Health NHS Trust started with completion of an application form which covered several domains such as specific benefits to the patient population, estimated use, cost, safety and environmental impact with supporting literature reviews. The approval came from the Integrated Care Board (ICB) after a positive application outcome and panel scrutiny. The ICB is a statutory NHS organisation responsible for developing a plan for meeting the health needs of the population, managing the NHS budget and arranging for the provision of health services in the Integrated Care System area. Within this, the Formulary and Pathways Group (FPG) processes and reviews all new drug applications, analyses and articulates the impact of new drug introductions providing a shared platform to help reduce inequity in access to medicines. Within the Trust, the Lead pharmacist managed this process and collaborated with the wider ICB for the FPG, ensuring the application was dealt with through the correct process, with an understanding of the impact of introductions on local services. It must be remembered that each Trust will have varying requirements in the approval process.
Acknowledgements
We would like to thank all the staff in the Special Care Dentistry team, the anaesthetic team and the theatre staff at the Royal London Hospital which contributed to the successful execution of this case. We would like to particularly thank Stacey Clough for her advice and summary of the remimazolam approval process at Barts Health NHS Trust.
Conflict of interest
The authors declare no conflict of interest in this paper.
References
1. Bradley N. Too old to sedate: How old is too old? Dental Update. 2021; 48:106–13.
2. Rockwood K. A global clinical measure of fitness and frailty in elderly people. Canadian Medical Association Journal. 2005; 173: 489–95. DOI: 10.1503/cmaj.050051
3. Rockwood K, Theou O. Using the Clinical Frailty Scale in Allocating Scarce Health Care Resources. Canadian Geriatrics Journal. 2020; 23: 254–9. DOI: 10.5770/cgj.23.463
4. Hoogendijk E O, Afilalo J, Ensrud K E, Kowal P, Onder G, Fried L P. Frailty: implications for clinical practice and public health. The Lancet. 2019; 394:1365–75. DOI: 10.1016/S0140-6736(19)31786-6
5. Pier Professional Ltd. Tizard Learning Disability Review Health inequalities and people with learning disabilities in the UK. 2011. Online information available at http://complexneeds.org.uk/modules/Module-4.1-Working-with-other-professionals/All/downloads/m13p020c/emerson_baines_health_inequalities.pdf(accessed June 2024).
6. Remimazolam for intravenous conscious sedation for dental procedures. Intercollegiate Advisory Committee for Sedation in Dentistry, 2023.
7. Kim K M. Remimazolam: pharmacological characteristics and clinical applications in anesthesiology. Anesthesia and Pain Medicine 2022; 17: 1–11.
8. Noor N, Legendre R, Cloutet A, Chitneni A, Varrassi G, Kaye A D. A comprehensive review of remimazolam for sedation. Health Psychology Research [Internet] 2021; 9: 24514. DOI: 10.52965/001c.24514
9. Pambianco D J, Cash B D. New horizons for sedation: The ultrashort acting benzodiazepine remimazolam. Techniques in Gastrointestinal Endoscopy 2016; 18: 22–8. DOI: 10.1016/j.tgie.2016.02.004/
10. Byfavo | European Medicines Agency. Online information available at https://www.ema.europa.eu/en/medicines/human/EPAR/byfavo (accessed May 2024).