Self-help resources incorporating cognitive behavioural techniques for patients with dental phobia: what’s available?
J. Hare DHealthPsy CPsychol AFBPS*1
T. Newton BA PhD CPsychol CSci AFBPsS FHEA2
1Consultant Health Psychologist, Dental Psychology Service, Guy’s and St Thomas’ NHS Foundation Trust and SAAD Editorial Board Member
2Professor of Psychology as Applied to Dentistry, King’s College London
*Correspondance to: Jennifer Hare
Email: Jennifer.Hare@gstt.nhs.uk
Hare J, Newton T. Self-help resources incorporating cognitive behavioural techniques for patients with dental phobia: what’s available? SAAD Dig. 2024: 40(II): 128-132
The launch of the new NHS England Clinical Standards for Dental Anxiety Management1 at the beginning of last year demonstrates a significant shift from the formerly titled Service standards for Conscious Sedation in a primary care setting. The clinical guide now includes a range of approaches which comprise behavioural techniques as both a stand-alone anxiety management strategy or as a complementary approach to support conscious sedation and general anaesthesia. The guide makes the important distinction between ‘trait anxiety’ (the more enduring apprehension concerning dental treatment that a person generally feels when contemplating, or engaging with, dental treatment) and ‘state anxiety’ (the individual’s degree of concern at a specific point in time when faced with a particular aspect of dental treatment such as local anaesthetic injections). This distinction is important since approaches to managing the two forms of anxiety may differ.
While conscious sedation and general anaesthesia offer an invaluable approach to provide dental treatment with increased comfort and reduced anxiety to individuals, there is also an appreciation that, when used in isolation, they may not target the underlying fear or trait anxiety. Therefore, opportunities to integrate pharmacological interventions alongside approaches based on cognitive behavioural (CB) techniques may afford the prospect to work on both state and trait anxiety simultaneously, supporting a rehabilitation model of dental fear.2
In recognition of this, the authors published an article in the 2018 SAAD Digest on Cognitive Behavioural Therapy (CBT) services and training options in the UK for dental professionals.3 However, since then a number of self-help CBT guides have become available to support patients and their dental teams which provide dental anxiety management interventions informed by CB principles and techniques. These resources support the implementation of some of the more advanced interventions referenced in the new standards1 which include the use of communication tools to support patient care.
This article aims to briefly outline two resources currently available for children and adults and consider their application for dental anxiety management.
1. Your teeth, you are in control
Produced by a team of experts in the field under the leadership of Sheffield Teaching Hospitals NHS Foundation Trust with collaboration between Kings College London, University of Reading, University of Glasgow and Five Areas Ltd, Your teeth, you are in control is a self-help CBT-based resource for young people (aged 9 to 16 years), with supplementary resources for parents and dental teams.4
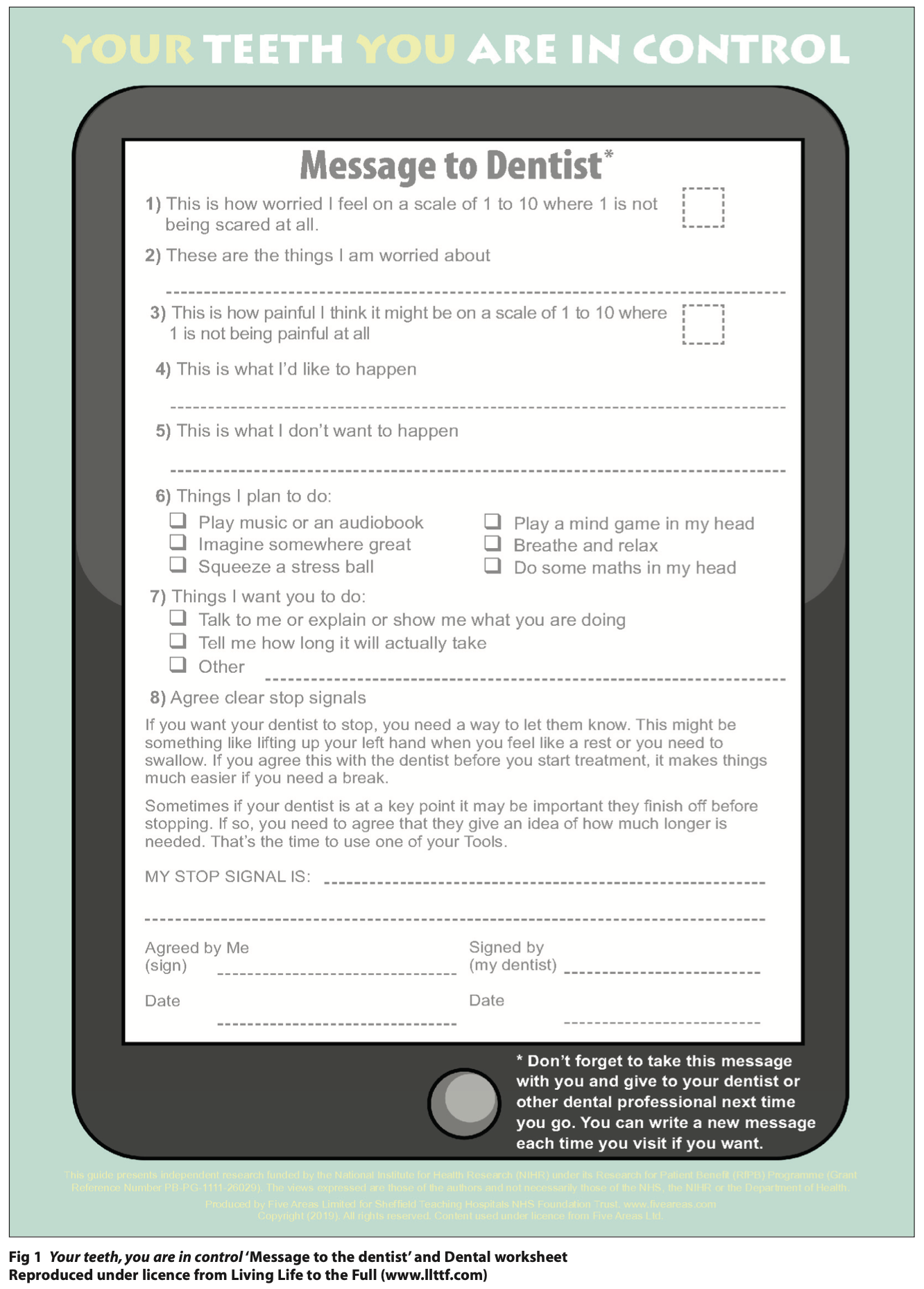
The authors suggest it is used with young people experiencing mild to moderate trait dental anxiety requiring non-urgent treatment. It is written to support the provision of a course of treatment with information on the dental setting, some basic dental procedures and specific tools and strategies to manage the physical sensations of anxiety. It also includes access to valuable resources to increase children’s sense of control including ‘Message to the dentist’ (Figure 1) which also facilitates enhanced communication between the child and the dental team, as well as a ‘stop signal signed agreement’. These are evidence-based techniques shown to reduce anxiety and distress in the dental setting.5,6 The guide also provides opportunities for the child and family to think about what went well at each visit, providing feedback on positive coping, an evidence-based CB-technique to support anxiety management in children.6 A full step-by-step process of how to implement the self-help guide is outlined in the BDJ Team article by Zoe Marshman,4 along with information on accompanying materials and guides to support parents / guardians and dental teams.
While the content and components of the self-help guide all hinge upon evidence-based CB-techniques, the guide itself was created as part of a collaborative research study with patient and public involvement.7 This preliminary investigation demonstrated encouraging results for the 48 children (out of 56 initially recruited) who completed the study, which comprised three dental treatment visits and pre- and post-treatment questionnaires.
Self-reported dental anxiety significantly reduced and health-related quality of life significantly increased following the use of the self-help guide with 60% of young people reporting feeling ’a lot less worried’ about visiting the dentist. The study further demonstrated high levels of acceptability of the self-help guide among young people and stakeholders, with recommendations to run a full randomised controlled trial (RCT) which is currently underway.
The CALM trial protocol is a four-year RCT being run across 30 primary care dental sites including general dental practices and primary dental community clinics across some of the most deprived areas in the UK with higher than average caries rates. The aim of the RCT is to establish the clinical and cost-effectiveness of the self-help CBT guide8 and we look forward to seeing the results in due course.
In addition to these research studies, a service evaluation published in 2019 reported encouraging findings on the use of the guide in a single general dental practice.9 Statistically significant reductions in dental anxiety reported using the Children’s Experiences of Dental Anxiety Measure (CEDAM) were seen within the evaluation’s 84 included young patients, with a mean age of 10.9 years old. This service evaluation demonstrates the ‘real-world’ applicability of the resource.
At present Your teeth, you are in control and the accompanying user-friendly resources are available to purchase in paper copy via the University of Sheffield website17 and the single-page ‘Message to the dentist’ is currently available to download for free (in a number of languages) via the Living Life to the Full (LLTTF) website.18 To learn more about the intervention and the resources, please visit these two websites.
2. Getting the dental care you need: getting through an urgent dental appointment
This CBT-based self-help book which is available both in printed form or online (Figure 2) is written for people with dental fear who now require urgent dental treatment and who may be in pain or have other urgent symptoms.10 Written by experts in dentistry and CBT, this practical resource teaches key skills to help people experiencing dental anxiety. It provides a structure of intervention for dental practitioners and teams wanting to support their patients, as well as for patients wanting to learn anxiety-management techniques they can use themselves or to help support a conversation with their dentist.
The content covers what might have caused dental anxiety onset and supports the learning of five strategies to manage dental fear in order to get through an urgent dental appointment.
These strategies consist of:
- Using topical numbing gel before an injection
- Agreeing start / stop signals
- Learning calm-controlled breathing
- Techniques to shift focus to the whole body and
- Listening to music or audiobooks.
There is also a specific section on ‘getting though a tooth extraction’ to prepare an individual by advising what to expect. In addition, the book aims to support the patient to communicate their dental anxiety fears to their dental practitioner and state how they wish to self-manage their anxiety during the treatment. Using the ‘dental care agreement’ (similar to the principles of ‘Message to the dentist’ outlined in the child-oriented resource) the two-page document is jointly reviewed and signed, with a commitment to support the patient’s choices and preferences agreed and the patient and clinician working together for an effective treatment outcome. The agreement helpfully includes a ‘my emergency dental kit’ checklist of treatment preferences to be agreed at the appointment which affords a greater sense of patient choice and control; vital ingredients in dental anxiety management.11
The authors suggest that the book can be both read as a standalone self-help guide for patients which can be applied in their own appointments or could be provided with support from dental teams.
While there are no specific research studies evaluating the use of this guide in practice as yet, the principles and evidence base of CBT are well-documented for dental fear and anxiety.12-16
At present, the Getting the dental care you need: getting through an urgent dental appointment book is available to purchase via the Living Life to the Full (LLTTF) website,18 where more information is available on how to use the resource, supporter notes and training information.
Final thoughts and conclusion
These two CBT-informed resources provide an opportunity for patients and practitioners to incorporate valuable CB-techniques into their dental anxiety management approach. They provide a user-friendly way to support both the patient and the dental team apply the techniques in practice, without necessarily completing specific training in CBT per se. It is important to note that using these resources in a standalone fashion cannot be considered as delivering a full course of CBT, as this requires appropriate training and cannot be used as a one-off, ad hoc technique.3
As we await the implementation guidance for the new Clinical standards for dental anxiety management, these resources, along with low level behavioural management techniques, provide a helpful approach to utilise in primary care settings. The authors appreciate the time required to incorporate these approaches effectively and it is sincerely hoped that this will be duly considered in the commissioning of services across all tier levels of dental care provision. Indeed, the concept of allowing for longer appointments is included in the new standards’ appendix1 where, over time as trust and rapport are built and dental anxiety reduced, working towards care delivery in standard appointment times might be a more realistic and achievable goal.
Figures
References
1. NHS England (2023). Clinical standards for dental anxiety management. Available from: https://www.england.nhs.uk/long-read/clinical-guide-for-dental-anxiety-management/
2. Newton T, Gallagher J, Wong F. The care and cure of dental phobia: the use of cognitive behavioural therapy to complement conscious sedation. Faculty Dental J 2017; 8: 160-163.
3. Hare J, & Newton J T. Cognitive Behavioural Therapy (CBT) for dental phobia: services and training options for dental professionals. SAAD Dig 2018; 34; 69-71.
4. Marshman, Z. Your teeth you are in control. BDJ Team 2017; 4: 15-17.
5. Richardson P H, Black N J, Justins D M, Watson R J. The use of stop signals to reduce the pain and distress of patients undergoing a stressful medical procedure: an exploratory clinical study. Br J Med Psychol 2009; 72: 397–405.
6. Pickrell J E, Heima M, Weinstein P, Coolidge T, Coldwell S E, Skaret E, Castillo J, Milgrom P. Using memory restructuring strategy to enhance dental behaviour. Int J Paediatr Dent 2007; 17: 439–448.
7. Porritt J, Rodd H, Morgan A, Williams C, Gupta E, Kirby J, Creswell C, Newton T, Stevens K, Baker S, Prasad S, Marshman Z. Development and Testing of a Cognitive Behavioral Therapy Resource for Children's Dental Anxiety. JDR Clin Trans Res 2017; 2: 23–37.
8. Bux S, Porritt J, Marshman Z. (2019). Evaluation of Self-Help Cognitive Behavioural Therapy for Children's Dental Anxiety in General Dental Practice. Dent J (Basel) 2019; 7: 36.
9. Marshman Z, Rodd H, Fairhurst C, Porritt J, Dawett B, Day P, Innes N, Vernazza C, Newton T, Ronaldson S, Cross L, Ross J, Baker S R, Hewitt C, Torgerson D, Ainsworth
H. The CALM trial protocol: a randomised controlled trial of a guided self-help cognitive behavioural therapy intervention to reduce dental anxiety in children. Trials 2023; 24: 15.
10. Williams C, Campbell C, Johnston E, Newton T. Getting the dental care you need: Getting through an urgent dental appointment. Clydebank: Five Areas Ltd, 2023
11. Wardle J. (1982). Management of dental pain. York: Paper presented at British Psychological Society.
12. Öst L, Skaret E. Cognitive Behaviour Therapy for Dental Phobia and Anxiety. London: Wiley, 2013.
13. Kvale G, Berggren U, Milgrom P. Dental fear in adults: a meta-analysis of behavioural interventions. Community Dent Oral Epidemiol 2004; 32: 250-264.
14. Wide Boman U, Carlsson V, Westin M, Hakeberg M. Psychological treatment of dental anxiety among adults: a systematic review. Eur J Oral Sci 2013; 121: 225-234.
15. Kani E, Asimakopoulou K, Daly B, Hare J, Lewis J, Scambler S, Scott S, Newton J T. Characteristics of patients attending for Cognitive Behavioural Therapy at one specialist unit for dental phobia in the UK and outcomes of treatment. Br Dent J 2015; 219: 501-506.
16. Porritt J, Jones K, Marshman Z. Service evaluation of a nurse-led dental anxiety management service for adult patients. Br Dent J 2016; 220: 515-20.
Websites:
17. University of Sheffield: https://www.sheffield.ac.uk/dentalschool/research/person-centred-population/child-dental-anxiety/resources (accessed 01/05/24).
18. Living Life to the Full (LLTTF) https://llttf.com/product/getting-the-dental-care-you-need/ (accessed 01/05/24).