Please click on the tables and figures to enlarge
The effect of remimazolam on a Parkinson’s patient
S. Madaan*1 BDS (Lond), MFDS RCS (Ed), General dentist with a special interest in restorative and surgical dentistry, St Johns Dental Practice, Oxford, OX1 2LH.
A. Harris2 BDS (Lond), DPDS, General dentist, visiting sedationist and SAAD accredited mentor, London, The Dentist Salisbury, SP1 2LH.
*Correspondence to: Dr Sita Madaan
Email: drsitamadaan@gmail.com
Madaan S, Harris A. The effect of remimazolam on a Parkinson’s patient. SAAD Dig. 2024: 40(II): 124-127
Case Summary
A 63-year-old lady who is 5 ft 4 in and weighs 66 kg was diagnosed with Parkinson’s disease in 2016. Sedation with remimazolam was used with the aim of alleviating the patient’s fears so that we could remove her poor prognosis teeth and perform socket preservation in the upper left quadrant with the view to placing dental implants in the future. We found that using remimazolam enhanced her involuntary movements due to Parkinson’s disease, with each dose administered.
Patient details
Gender: Female
Age at start of treatment: 62
Pre-treatment assessment
The patient presented with a left-sided swelling of the buccal space relating to two upper retained roots, not affecting the eye, and a toothache of two weeks. The patient stopped caring about her dental health after she was diagnosed with Parkinson’s disease in 2016 and started to neglect her dentition. She has started to feel self-conscious of her teeth but is extremely nervous of the dentist and has only presented because she had been suffering with pain for two weeks and had developed an abscess relating to some retained roots.
Relevant medical history
The patient is an ASA II. She was diagnosed with Parkinson’s disease in 2016. The patient also suffers from epilepsy and has been diagnosed as having grand mal seizures, although she had experienced a petit mal seizure in the last year. She has also been diagnosed with hypothyroidism. Overall, the patient is mobile, but says she is stiff in the morning and ok with stairs.
Medications
- Co-careldopa 50mg: primarily used to manage the symptoms of Parkinson's disease, however, it does not slow down the disease or prevent it from worsening
- Ropinirole 100mg a day: used to treat the symptoms of Parkinson's disease and restless legs syndrome - it can improve symptoms like shaking (tremors), slowness and stiffness
- Epilim 4mg bd: for epilepsy
- Levothyroxine 100µg od
- The patient also has a codeine allergy.
Previous sedation history
The patient has never been sedated before and has a BMI of 25. Her alcohol intake is 18 units per week with no history of taking benzodiazepines or recreational drugs. Her pre-operative blood pressure was 120/78.
Dental history
Irregular attender, has not attended for over 10 years.
Clinical examination
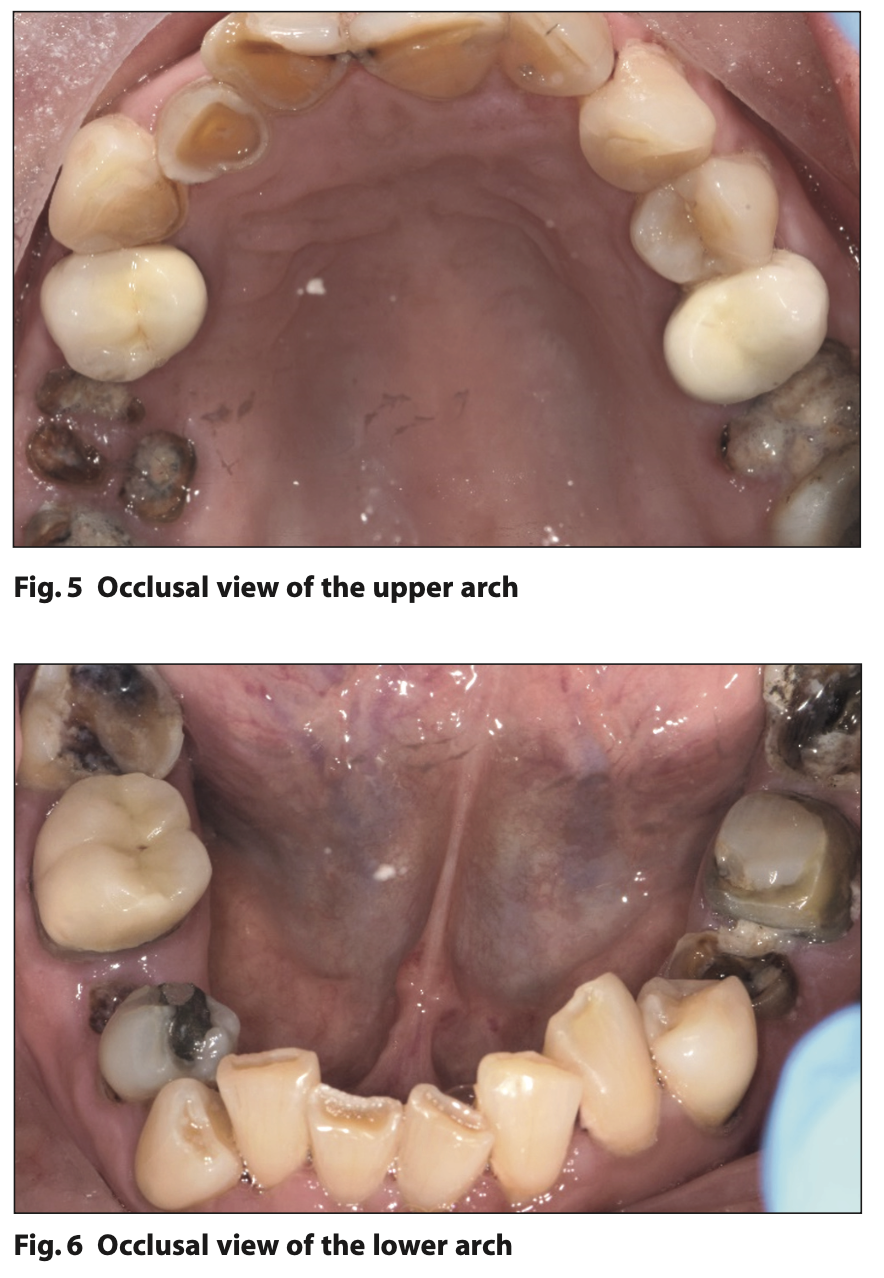
The patient had some trismus, not relating to dental infection. Several fractured teeth were seen with heavy evidence of parafunction and her muscles of mastication were tender because of this. There was evidence of heavy palatal erosion due to dietary acids, which the patient was unaware of. Calculus, plaque, and gingivitis were present throughout the mouth.
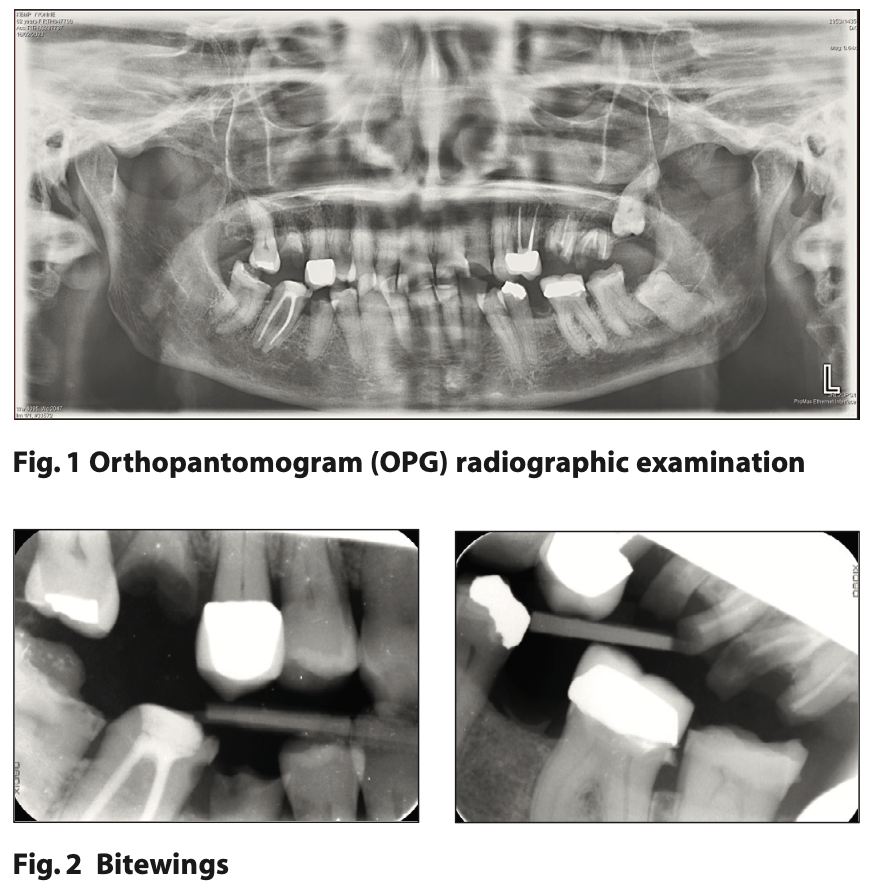
Bitewings and an OPG were taken for a full assessment of the patient’s dentition which showed:
LR7 is fractured and requires vitality testing and then cuspal coverage.
LR6 is a root filled tooth which has been prepared for a crown and will require a new crown.
LR5 is fractured with deep caries and has been recommended for extraction.
LL5 retained root recommended for extraction.
UR6 is a root fragment and requires extraction.
UR2-UL2 are fractured. Wear and exposed dentine can be seen clinically.
UL4 is a metal post crown with a questionable long-term prognosis.
UL6 and UL7 are root filled retained roots with signs of periapical pathology around UL7.
UL8 LL8 are unerupted.
There is mild generalized horizontal bone loss with vertical bone loss around the UL6 retained root.
Pre-treatment photographs
Diagnostic summary
- Mild periodontitis (Stage 2 Grade A), which is active at present, with poor oral hygiene due to demotivation to look after oral health since onset of Parkinson’s disease.
- Buccal caries on the lower premolars.
- Retained roots which will require extraction. Multiple fractured teeth requiring cuspal coverage.
- Palatal wear of the upper anteriors and fractured upper and lower incisors due to erosion, attrition and tooth position.
- Post-extraction spaces which will require fixed, long-term space replacement to keep the bone stimulated and prevent bone loss from occurring in these areas.
Aims and objectives of treatment
- Stabilisation of oral hygiene and gingival inflammation
- Strengthening of enamel to reduce the risk of future decay and prevent tooth wear with high fluoride toothpaste
- Elimination of any causes of disease, and to bring about a state of health, function and self-confidence
- Alleviation of dental anxiety using treatment under IV sedation.
Treatment plan
- Prevention advice: oral hygiene to be reinforced with emphasis on motivating the patient to introduce interdental cleaning into her regime. To discuss use of plaque disclosing tablets to aid removal of biofilm. Duraphat toothpaste to be prescribed to strengthen enamel against decay and prevent further tooth surface loss, which is of multifactorial origin (attrition and erosion)
- Oral hygiene stabilisation with hygienist and periodontist involvement
- Extraction of poor prognosis teeth and socket preservation in the upper left region as the patient would like to consider fixed space replacement, in the form of dental implants, if her oral hygiene permits this in the future. The patent is aware of the risks associated with dental implants including peri-implantitis. This phase of treatment will be carried out under IV sedation using remimazolam, due to the better sedative profile than that of the current drugs, including rapid onset and offset of sedation and a predictable duration of action
- Caries stabilisation of lower premolars which require filling cervically
- Fractured teeth to have cuspal coverage restorations and post crown to be monitored
- Fractured anterior teeth and palatal exposed dentine to be repaired
- Patient is also a heavy bruxist and will need some form of protection at the end of treatment.
Treatment undertaken
- The initial presentation was as a new patient at an emergency appointment in February 2023 during which an assessment was carried out, a periapical radiograph (PA) was taken and referral for full mouth Orthopantomogram (OPG) made. Antibiotics were prescribed to prevent the further spread of infection and the patient was advised to return for a full mouth detailed clinical examination. Even though there were no signs of septicaemia or cellulitis, the patient’s reduced co-operation and compromised oral hygiene until this point was taken into consideration as a risk factor for further spread of infection.
- The patient then saw the periodontist and had multiple sessions with the hygienist every three weeks where disclosing tablets were used to aid oral hygiene instruction.
- She expressed her concerns about undergoing dental treatment and explained that she was nervous. We discussed the possibility of sedation, and she filled out an Indicator of Sedation Need form. Her pre-operative sedation score was 21 indicating a very high Modified Dental Anxiety Scale (MDAS) score. Given her underlying medical health and considering the treatment complexity this gave a score of ‘very high need’ for sedation.
- We elected to use remimazolam due to its superior properties over midazolam such as rapid induction, rapid recovery, and less respiratory depression.1 The patient then attended in May 2023 for extraction of all retained roots, UR5, UL6, UL7, LR5, LL5 and socket preservation in the upper left quadrant (ULQ). At this stage the drug was in its infancy for use in general dental practice sedation cases, as remimazolam was approved for use in dentistry in the UK in January 2023.
Treatment findings
A total of 17.5 mg of remimazolam was administered over the course of 1 hour 15 mins. An initial 5 mg dose was administered. With every subsequent 2.5 mg increment given the patient demonstrated jerky movements and signs of un-cooperation. Her legs started to jerk, and her jaw would clamp down which would impede the procedure but then she would settle down. A brief timeline of events is as follows:
11.54: Rapid induction of remimazolam (5 mg over 2 mins)
11.58: The patient did not like the administration of local anaesthetic
12.06: 2.5 mg administered, patient became unco-operative and was very jerky during the upper left quadrant extractions
12.28: 2.5 mg administered. The patient reported ‘this is a great experience’.
12.32: 2.5 mg administered. Bone grafting of the upper left quadrant.
12.36: The patient was much more relaxed.
12.42: Sutures placed and collagen plug.
12.53: Patient is relaxed during further suturing
13.00: 2.5 mg administered, patient is unco-operative again
13.10: Patient is more aware of what is going on
13.13: 2.5 mg administered
13.20: Patient did not like local anaesthetic (LA)
13.35: Patient was co-operative for extractions
13.49: Patient settled down and was more co-operative but was aware of treatment
13.55: Remaining lower surgical extraction was completed
14.00: Procedure finished
Long term treatment and future considerations
In future, we could consider giving a reduced dose over a longer administration period. However, reducing the duration of the drug use would make it unsuitable for long surgical types of procedures. It is worth considering that now that she has been reintroduced to dental work after several years, she may have a lower sedation score in future and may not need treatment under sedation going forward. Her next phase of treatment would be restorative and only when we come to implant placement may she feel a need to revisit the idea of sedation.
We could consider trying to manage her pre-operative anxiety using other relaxation techniques such as deep relaxation with diaphragmatic breathing or hypnotherapy2. We could also consider the use of midazolam as there are case reports to support the use of this drug to ease the symptoms of Parkinson’s disease.2
At present the patient is still mid-restorative phase due to a fall and subsequent hip injury, causing a delay in the completion of her treatment. The anterior restorative work which has been carried out so far was unremarkable and was undertaken under local anaesthetic with ease.
Discussion and reflection about case presented
As remimazolam was only approved for use in dentistry in UK in January 2023, the seditionist had limited experience of practical cases with this drug. In hindsight, she could have started with a lower induction dose and could have given lower top-up doses, as the patient swung from being co-operative to unco-operative immediately after top-up increments.
On a follow up phone call the next day, the patient reported that the sedation was ‘fabulous’, she didn’t remember anything about the treatment apart from the tail end of the appointment and the patient was much more co-operative at this point. She felt normal upon leaving the practice and was delighted with the outcome.
Oral surgery can be difficult in patients with chorea-like dyskinesia (involuntary movements) which is common in those on long-term levodopa medication for Parkinson's disease,3 and we know of no conclusive evidence to indicate whether conscious sedation with midazolam is effective in such cases. However, there are case reports of a patient in whom levodopa-induced chorea-like dyskinesia disappeared when midazolam was given intravenously for conscious sedation, so this drug could be preferred in such patients.3
References
1. Kim K M. Remimazolam: Pharmacological Characteristics and Clinical Applications in Anaesthesiology. Anesth Pain Med (Seoul) 2022; 17: 1–11.
2. Wang R, Huang X, Wang Y, Akbari M. Non-pharmacologic approaches in preoperative anxiety: a comprehensive review. Front Public Health 2022, 10: 852673.
3. Shibuya M, Hojo T, Hase Y, Fujisawa T. Conscious sedation with midazolam intravenously for a patient with Parkinson's disease and unpredictable chorea- like dyskinesia. Br J Oral Maxillofac Surg 2018; 56: 546-548.