Please click on the tables and figures to enlarge
Pilot video consultations to assess high BMI paediatric patients’ suitability for the provision of dental treatment under general anaesthesia at a Day Surgery Unit
B. Tailor BDS MSc1*
N. Seth FRCA2
N. Bhujel FDSRCS3
1Specialty Dentist, Department of Paediatric Dentistry, Guy’s and St Thomas’ NHS Foundation Trust, Guy’s and St Thomas’ NHS Foundation Trust, Westminster Bridge Road, London SE1 7EH
2Consultant Paediatric Anaesthetist, Anaesthetic Department, Evelina London Children’s Hospital and Guy’s and St Thomas’ NHS Foundation Trust, Westminster Bridge Road, London SE1 7EH
3Consultant in Paediatric Dentistry, Department of Paediatric Dentistry, Evelina London Children’s Hospital and Guy’s and St Thomas’ NHS Foundation Trust, Westminster Bridge Road, London SE1 7EH
*Correspondence to: Bina Tailor
Email: bina.tailor@gstt.nhs.uk
Tailor B, Seth N, Bhujel N. Pilot video consultations to assess high BMI paediatric patients’ suitability for the provision of dental treatment under general anaesthesia at a Day Surgery Unit. SAAD Dig. 2025: 41(I): 13-16
Key learning points
- Calculate BMI using the NHS BMI calculator: https://www.nhs.uk/health-assessment-tools/calculate-your-body-mass-index/calculate-bmi-for-children-teenagers
- Childhood obesity and associated comorbidities may impact a child's dental general anaesthetic journey
- Video consultation has a place for aiding preoperative planning for children with high BMI.
Abstract
Background
Childhood obesity is an increasing healthcare challenge as these children can have increased risk of peri-operative complications. Video consultations were introduced for children and young people between the ages of two and 16 years who were clinically overweight, with a body mass index (BMI) centile above 93. Suitability for treatment at the Guy’s and St Thomas’ NHS Foundation Trust Day Surgery Unit (DSU) was assessed using this pilot service. Patients assessed to be at high risk of complications were triaged to receive treatment at an in-patient general anaesthetic (GA) facility.
Aim
To enhance the safe delivery and recovery of GA for overweight paediatric patients requiring dental treatment.
Method
All children planned for dental treatment under GA with a BMI over 93, calculated using the NHS BMI calculator, and an ASA (American Society of Anesthesiology) classification score I or II were booked for a pre-general anaesthetic assessment via video consultation. We collected patient demographics and outcome in terms of whether their GA was suitable for a DSU or an in-patient setting.
Results
Twenty-seven patients had video consultations. Twenty patients were deemed suitable for GA at DSU and seven were treated in an in-patient setting. There were no adverse events under GA. New departmental protocols were implemented to signpost staff and patients to the options and pathways to access general anaesthetic care in the DSU or in-patient setting.
Conclusion
Video consultation can be a suitable alternative to face-to-face pre-operative assessment for high BMI paediatric patients.
Background
Childhood obesity is one of the biggest public health issues facing the United Kingdom.1 The definitions of being overweight or obese describe states where abnormal or excessive fat accumulation present a risk to health.2 Obesity increases the risk of developing a range of health conditions in childhood and later life, including heart disease, stroke, high blood pressure and diabetes.3 Obese children are much more likely to be obese adults.4
The body mass index (BMI) is a measure that uses patient height and weight to calculate a value used to predict an individual’s health and consequent risk of morbidity and mortality. The BMI calculation divides an adult's weight in kilograms by their height in metres squared. For children and young people aged between two and 16 years, the BMI calculation takes into account age and gender as well as height and weight. A child’s BMI is given as a ‘centile’. The centile number shows how their BMI compares with other children of the same age and sex as a percentage.5 According to the National Health Service (NHS) online BMI calculator,5 the following definitions have been given to a child’s and a young person’s weight according to their calculated BMI: underweight (on the 2nd centile or below), a healthy weight (between the 2nd and 91st centiles), overweight (91st centile or above) or very overweight (98th centile or above).
General anaesthesia is often required to provide dental treatment for children. Prior to this pilot service, if a paediatric patient had a BMI of 93rd centile or above and required dental treatment under GA at Guy’s and St Thomas’ NHS Foundation Trust (GSTT) they were placed on the in-patient pathway for their dental treatment in order to avoid the risk of peri-operative complications from obesity during a general anaesthetic. Medically compromised children, children with a significant disability, additional needs or who required post-surgery monitoring also followed the in-patient pathway for their dental GA. Fit and healthy children aged between two and 16 years who required dental treatment under GA followed an out-patient GA pathway in a Day Surgery Unit (DSU).
Consultation with senior anaesthetic and paediatric dentistry colleagues highlighted that the increasing prevalence of patients with a high BMI had resulted in the in-patient waiting list being under additional pressures. As the list increased, the potential wait for other patients requiring in-patient admissions eg those with additional needs and medically compromised children increased. It was felt that not all of the children who had a BMI above the 93rd centile required in-patient treatment. There was thus a possibility that they were waiting longer for their dental GA.
This pilot study involved the use of teledentistry to assess the suitability of overweight paediatric patients for dental treatment under GA in an in-patient or an out-patient facility. Teledentistry is defined as the provision of real time, online dental care to aid diagnosis, treatment planning, consultation and follow-up via electronic transmission from and to different sites.7,8 Two formats of teledentistry were implemented in this pilot:
1. Store and forward7,9
All new patients referred to the service underwent a face-face dental assessment. The completed outcomes e.g. medical history, clinical examination, special investigations, diagnosis, treatment plan and stage one consent for dental treatment and referral for treatment under GA were recorded on the GSTT Information Technology (IT) System at the Paediatric Dental Centre in St Thomas’ Hospital. This information is also accessible on the same GSTT IT System at the DSU at an alternate site within the Trust, Guy’s Hospital. An appointment for video consultation could thus be booked and the video consultation completed from the alternate site.
2. Video consultation7,9
Real time interaction via video consultation was booked via video calls. In the pilot, the video calls were approximately ten minutes in duration. The outcome of the video consultations determined whether the paediatric patient continued to follow the in-patient paediatric dental GA pathway or whether they were identified as safe to be transferred to an out-patient DSU setting for their dental treatment under GA.
Aim
To enhance the safe delivery and recovery of GA for overweight paediatric patients requiring dental treatment.
Method
The pilot was registered and approved by the Trust’s Clinical Governance team (ID number 14593). Video consultations were organised for all paediatric patients aged between two and 16 years planned for the delivery of dental treatment under GA with a BMI of 93rd centile and above and an ASA score of I or II. Initial treatment planning was completed between December 2021 and November 2022 at either a face-to-face paediatric consultant new patient clinic, follow up clinic assessment, paediatric consultant lead dental accident and emergency appointment or any of the joint multi-disciplinary clinics held at the paediatric dental facilities.
Video consultations took place from the DSU at Guy’s Hospital Tower Wing on Floor 23 over a period of 13 months from December 2021 to December 2022. The calls involved a Consultant Anaesthetist, a Consultant in Paediatric Dentistry, a member of the GA nurse recovery team and the paediatric patient with their parent or legal guardian in their home or their chosen environment. The platform used was the secure NHS Attend Anywhere service.10 The appointments were booked one week in advance of the appointment date when the availability of all members of the team was confirmed. The following assessments were carried out virtually:
- Confirmation of medical history and allergy status
- Mouth opening and neck movement
- Assessment of potential intravenous access sites
- Potential co-operation / behavioural issues
- Any requirement for pre-medication.
Results
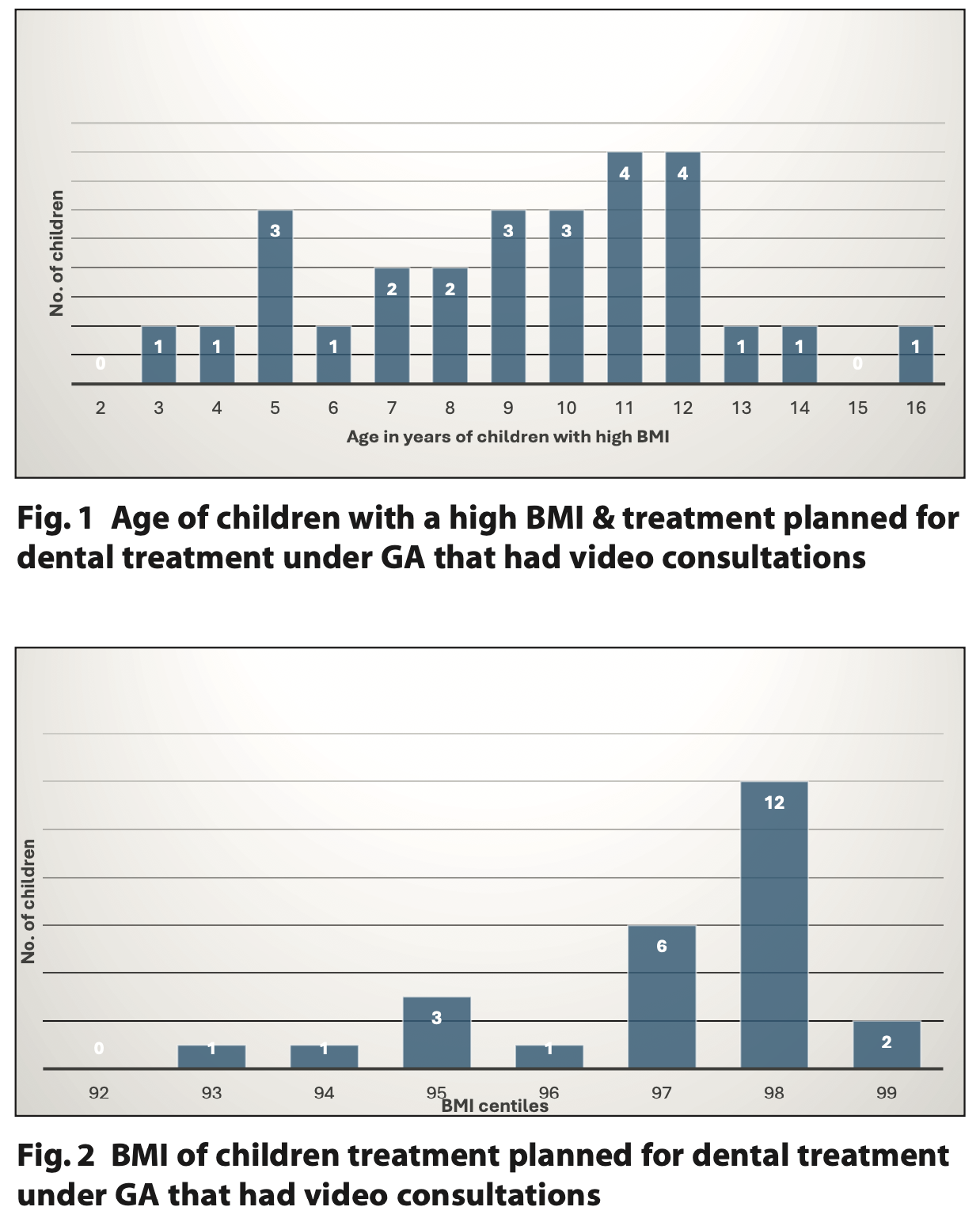
Twenty-seven video consultations were carried out. The average age of children seen via video consultation was 9 years 3 months (Figure 1). The mode BMI centile was the 98th centile for children seen via video consultation (Figure 2) and following both GA pathways.
Following the video consultation, 20 of these patients followed the out-patient GA pathway and seven, the in-patient GA pathway. The last out-patient GA case booked following a video consultation was completed January 2023. Two thirds of the cases on this pathway had dental oral rehabilitation including restorations and extractions. One third of the cases had dental extractions only. More than half (56%) of the children on the DSU pathway had an intravenous induction and under half (44%) had a gas induction. While on the out-patient GA waiting list, one family opted for their child to have the dental treatment delivered with local anaesthetic in the dental chair.
Children waited between six and 112 days between their video consultation and the date of their dental treatment under GA on DSU (Figure 3). The average waiting time was 32 days to first booking and 35 days where rebooking was required. Reasons for rebooking included the patient being unwell on the day of surgery, industrial action by nurses, patient not being brought to the appointment and family requests for rebooking due to pre-arranged holidays.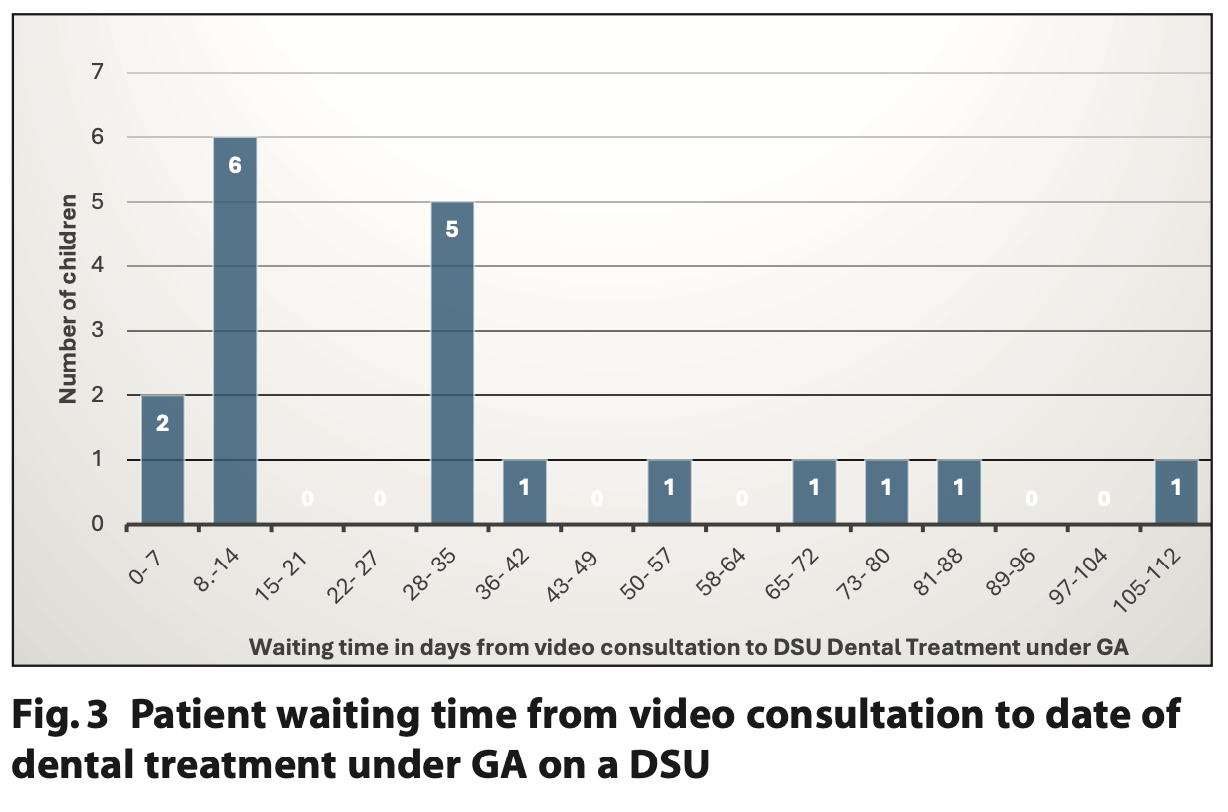
Following four hours and thirty minutes of pre-anaesthetic video consultations, the in-patient dental GA waiting list was reduced by 20 patients. There was safe delivery and recovery from GA for all 19 children who were overweight and who underwent dental treatment via the out-patient DSU dental GA pathway. No adverse events were recorded.
Discussion
This service evaluation has demonstrated the usefulness of teledentistry via a secure and suitable platform to assess the suitability of children for planned dental GA. The video consultations were piloted at a time when dental service providers were dealing with the backlog of patients following the impact of the COVID-19 pandemic in 2020, when all routine dentistry ceased, including elective dental treatment under GA.11 In the south east of England 1,456 children had their GA dental extraction appointments cancelled between the 20th March and 30th June 2020 due to the COVID-19 pandemic.12 In addition to reducing a paediatric in-patient waiting list and waiting times, video consultations eliminated the challenges of swab testing and self- isolation required prior to attending hospital appointments.
The new departmental guidelines implemented involve categorisation of overweight paediatric patients with an ASA I or II score requiring a dental GA into two age categories. The first category included children aged between two and 12 years of age whilst the second category included children aged over 12 years. For both categories, the BMI is calculated by using the equation weight (in kilograms) divided by height (in metres squared). For the two to 12-year-olds the BMI value calculated is checked against the WHO gender-specific centile chart. If the patient is below the 99th centile, the child follows the DSU GA pathway and those whose BMI is in the 99th centile and above follow the in-patient GA pathway. For children aged over 12 years of age, the BMI value calculated was plotted on the gender-specific BMI chart. A score of 27 and below means the child is allocated to the DSU GA pathway whilst a score of 28 and above means the child is placed on the in- patient GA pathway.
Childhood obesity is an increasing healthcare challenge and dental GA teams must be aware of the potential challenges that overweight and very overweight children pose. The National Child Measurement Programme (NCMP) is an annual, nationally mandated public health programme in England that measures the height and weight of children in Reception (aged four to five years) and Year 6 (aged ten to 11 years). The aim of the programme is to assess overweight and obesity levels in children within primary schools.13 It provides the data for the child excess weight indicators in the Public Health Outcomes Framework and is part of the government’s approach to tackling child obesity. The Royal College of Paediatrics and Child Health conducts population monitoring studies using definitions relating to a child’s calculated BMI. A child is said to be underweight if they are on the 2nd centile or below. Below the 85th centile is defined as a healthy weight. A BMI between the 85th and 95th centile would categorise a child as overweight and those above the 95th centile as being very overweight or obese.14 These are the definitions also used by NCMP.
NCMP figures for childhood obesity for the past five years show a general rise in obesity. For children in both Reception and Year 6, obesity prevalence is higher in boys than in girls. For children living in the most deprived areas of England, obesity prevalence for Reception-aged children is, and has been, twice as high when compared with those living in the least deprived areas of England for the past four consecutive years. This difference is three times more likely by Year 6.15,16,17,18
On the 1 March 2024, the WHO released the following key facts relating to overweight and obesity associated with children:
- In 2022, 37 million children under the age of five were overweight
- Over 390 million children and adolescents aged five to 19 years of age were overweight in 2022
- The prevalence of overweight (including obesity) among children and adolescents aged five to 19 years has risen dramatically from just 8% in 1990 to 20% in 2022
- The rise has occurred similarly among both boys and girls: in 2022 19% of girls and 21% of boys were overweight
- While just 2% of children and adolescents aged five to 19 years were obese in 1990 (31 million young people), by 2022, 8% of children and adolescents were living with obesity (160 million young people).19
Children and adolescents with obesity are around five times more likely to become obese adults with associated increases in morbidity and mortality. Obesity has direct healthcare and indirect social consequences, contributing significantly to economic burden. Children with obesity more often have comorbidities, such as hypertension, type 2 diabetes mellitus, asthma, obstructive sleep apnoea (OSA), fatty liver, and gastro-oesophageal reflux disease, which all increase peri-operative risk.20 Childhood obesity and excess weight are also significant health issues for children and their families. There can be serious implications for a child’s physical and mental health, which can continue into adulthood. The number of children with an unhealthy and potentially dangerous weight is a national public health concern.21
Managing the obese child is becoming a common scenario for the anaesthetist as obese children are more prone to developing peri-operative respiratory adverse events associated with obesity. The most common peri-operative respiratory adverse events in obese children undergoing elective general surgery include oxygen desaturation, difficult mask ventilation, airway obstruction, and bronchospasm especially at younger ages. Venous access can be more difficult and drug distribution is altered.22,23 A study performed by the Paediatric Anaesthesia Trainee Research Network entitled ‘Prevalence of PErioperAtive CHildhood obesity (PEACHY) in children undergoing general anaesthesia’ was the first prospective, multicentre, observational cohort study to estimate UK paediatric obesity prevalence peri-operatively. It revealed that 24% of children requiring surgery in 102 UK hospitals were overweight or obese. The study also concluded that the majority of hospitals did not routinely measure BMI or offer dietary and lifestyle advice to overweight children and should be strongly encouraged to do so in the future.20 How a patient’s BMI affects patient care, however, should be carefully considered. The BMI does not differentiate between muscle and fat mass. Some children may have higher muscle mass or bone density affecting their BMI. Hence the fully comprehensive assessment of medical history, allergy status, mouth opening, neck movement, assessment of potential intravenous access sites, deposition of adipose tissue in the upper airway and torso, potential co-operation / behavioural issues and any requirement for pre-medication is required as part of the pre-anaesthetic assessment. The Mid Yorkshire Teaching NHS Trust investigated whether overweight children with a BMI of the 91st centile and above required additional anaesthetic time on their exodontia list. Their results showed that the difference in anaesthetic time (average induction time and average recovery time in theatre) was not clinically significant between the overweight and healthy weight children in the two to 16 years age group. In their sample, 19.5% of the children (n = 123) were overweight.24 Their aim was to enhance safe delivery and recovery of GA for this cohort of paediatric patients requiring dental treatment under GA by emphasising overweight prevention and weight management. Their study highlighted the role dental teams could play in screening for obesity and signposting to weight management interventions.24,25
In October 2023, GSTT migrated all patient records and bookings to an integrated electronic noting system (EPIC). The aspiration is the development of a pathway for paediatric dental patients identified to have a high BMI, to be directed to their general practitioner (GP) to assist with weight management alongside staff training on navigating this sensitive conversation. Similar work has been carried out by the Paediatric Dental Department at the Royal National ENT and Eastman Dental Hospitals.26 The importance of linking BMI calculations recorded at new patient or follow up patient assessments for children and young adults is also highlighted as an aim in the ‘Making Every Contact Count: Consensus’ statement.27 This approach would seize each and every opportunity to provide dietary and lifestyle advice, along with referral to their GP or paediatrician where appropriate.
Future improvements to this service could include a sustainability impact analysis for the video consultations. This would include a calculation of the total travel miles saved as the twenty-seven families were not required to physically attend an appointment. Unfortunately, patient identifiable information including post codes were not collected in this pilot study. A patient satisfaction survey on the pilot video consultations would also allow qualitative assessment of patient or proxy reported outcomes.
Conclusion
Video consultations were a suitable alternative to face-to-face pre-operative assessments for overweight paediatric patients. New departmental guidelines on allocating overweight and obese paediatric patients to the in-patient and DSU out-patient dental GA pathway have been implemented and will continue to be appraised for efficacy, environmental sustainability and patient safety.
References
1. Cheung R, Matthews-Jones G, McKeown R, Shah R. State of Child Health – Healthy Weight. Royal College of Paediatrics and Child Health: London; 2020 Online information available at https://stateofchildhealth.rcpch.ac.uk/evidence/prevention-of-ill-health/healthy-weight/#page-section-3 (Accessed 12 March 2024).
2. World Health Organization. Obesity. Online information available at https://www.who.int/health-topics/obesity#tab=tab_1 (Accessed 12 March 2024).
3. Reilly J J, Methven E, McDowell Z C et al. Health consequences of obesity. Arch Dis Child 2003; 88: 748-52.
4. Simmonds M, Llewellyn A, Owen C G, Woolacott N. Predicting adult obesity from childhood obesity: a systematic review and meta-analysis. Obes Rev 2016; 17 : 95-107.
5. NHS UK. Calculate your body mass index (BMI) for children and teenagers. 2023. Online information available at https://www.nhs.uk/health-assessment-tools/calculate-your-body-mass-index/calculate-bmi-for-children-teenagers/ (Accessed 12 March 2024).
6. Owen J, John R. Childhood obesity and the anaesthetist. Contin Educ Anaesth Crit Care Pain 2012; 12 : 169-75.
7. Wallace C K, Schofield C E, Burbridge L A L, O’Donnell K L. Role of teledentistry in paediatric dentistry. Br Dent J 2021; 230: doi.org/10.1038/s41415-021-3015-y. Online information available at https://www.nature.com/articles/s41415-021-3015-y (Accessed 12 March 2024).
8. Chen J-W, Hobdell M H, Dunn K, Johnson K A, Zhang J. Teledentistry and its use in dental education. J Am Dent Assoc 2003; 134: 342-6.
9. Jampani N D, Nutalapati R, Dontula B S K, Boyapati R. Applications of teledentistry: A literature review and update. J Int Soc Prev Community Dent 2011; 1: 37-44. Online information available at doi: http://dx.doi.org/10.4103/2231-0762.97695 (Accessed 12 March 2024).
10. NHS England. Video Call Management. Online information available at https://england.nhs.attendanywhere.com/ (Accessed 12 March 2024)
11. Royal College of Surgeons Faculty of Dental Surgery. Recommendations for paediatric dentistry during the recovery phase of the COVID-19 pandemic – June 2020. Online information available at https://www.rcseng.ac.uk/-/media/Files/RCS/FDS/Guidelines/v3_Recomndations-for-Paediatric-Dentistry_June2020.pdf
12. Elsherif N, Lewney J, John J H. Impact of cancelled general anaesthetic dental extraction appointments on children due to the COVID-19 pandemic. Community Dent Health 2021; 38: 209-14.
13. NHS Digital. National Child Measurement Programme – Defining overweight and obesity in children. Online information available at https://digital.nhs.uk/services/national-child-measurement-programme/#defining-overweight-and-obesity-in-children (Accessed 12 March 2024).
14. Royal College of Paediatrics and Child Health. State of Child Health in the UK. Online information available at https://stateofchildhealth.rcpch.ac.uk/ (Accessed 12 March 2024).
15. NHS Digital. National Child Measurement Programme, England 2019/20 School Year. Online information available at https://digital.nhs.uk/data-and-information/publications/statistical/national-child-measurement-programme/2019-20- school-year (Accessed 12 March 2024).
16. NHS Digital. National Child Measurement Programme, England 2020/21 School Year. Online information available at https://digital.nhs.uk/data-and-information/publications/statistical/national-child-measurement- programme/2020-21-school-year (Accessed 12 March 2024).
17. NHS Digital. National Child Measurement Programme, England, 2021/22 School Year. Online information available at https://digital.nhs.uk/data-and-information/publications/statistical/national-child-measurement- programme/2021-22-school-year (Accessed 12 March 2024)
18. NHS Digital. National Child Measurement Programme, England, 2022/23 School Year. Online information available at https://digital.nhs.uk/data-and-information/publications/statistical/national-child-measurement- programme/2022-23-school-year (Accessed 12 March 2024).
19. World Health Organisation. Obesity and overweight. Online information available at https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (Accessed 15 June 2024).
20. Burton Z A, Lewis R, Bennett T, McLernon D J, et al Prevalence of PErioperAtive CHildhood obesitY in children undergoing general anaesthesia in the UK: a pros-pective, multicentre, observational cohort study. Br J Anaesth. 2021; 127: 953-961.
21. Office for Health Improvement & Disparities. Guidance - Childhood obesity: applying All Our Health. Updated 7 April 2022. Online information available at https://www.gov.uk/government/publications/childhood-obesity-applying-all-our-health/childhood-obesity-applying-all-our-health (Accessed 12 March 2024).
22. Marjanovic V, Budic I, Breschan C. Perioperative respiratory adverse events during ambulatory anesthesia in obese children. Ir J Med Sci. 2022 ; 191:1305–1313.
23. El-Metainy S, Ghoneim T, Aridae E, et al. Incidence of perioperative adverse events in obese children undergoing elective general surgery. Br J Anaesth. 2011;106 :359–363.
24. Jones H, McDerra E, Nichol R. Childhood obesity and dental general anaesthetics [poster]. Int J Paed Dent 2023; 33 (S2): P43. Online information available at https://onlinelibrary.wiley.com/doi/full/10.1111/ipd.13107 (Accessed 12 March 2024).
25. Daley A J. Time to get our teeth into reducing obesity: should dentists screen and deliver interventions to reduce obesity in the population? Br Dent J 2022; 232 : 78-9.
26. Chan K H C, Dunkley S, Devalia U. Three-cycle audit to assess the compliance of a body mass index pathway [poster]. Int J Paed Dent 2023; 33 (S2): P21. Online information available at https://onlinelibrary.wiley.com/doi/full/10.1111/ipd.13107 (Accessed 12 March 2024).
27. Public Health England. Making Every Contact Count (MECC): Consensus statement. NHS England; 2016. Online information available at https://www.england.nhs.uk/publication/making-every-contact-count-mecc-consensus-statement/ (Accessed 12 March 2024).