Please click on the tables and figures to enlarge
Challenges and considerations in dental treatment of patients with psychogenic non-epileptic seizures: a review and case study
H. Patel*1
C. Boynton2
1Senior Dental Officer
2Consultant Special Care Dentistry
Salaried dental service, Royal Devon University Healthcare NHS Foundation Trust
Correspondence to: Mrs Hiral Patel
Email: Hiralpatel1@nhs.net
Patel H, Boynton C. Challenges and considerations in dental treatment of patients with psychogenic non-epileptic seizures: a review and case study. SAAD Dig. 2025: 41(I): 3-7
Key learning points
- Understanding the diverse manifestations of PNES, its epidemiology, and associated comorbidities
- Clinical considerations for dental management and conscious sedation in patients with PNES
- Case study describing episodes of PNES during conscious sedation
Abstract
Psychogenic non-epileptic seizures (PNES) or functional or dissociative seizures are a common subtype of functional neurological disorder. These seizures may present as dissociation, blackouts, collapse or closely resemble epileptic seizures without the changes in electrical activity in the cortex. Patients with these seizures present with unique challenges in management of their dental treatment because of their associated co-morbidities and complex presentation. They are often referred to community or hospital dental settings to manage their dental care. Although non-epileptic seizures are increasingly common, there is a lack of evidence for their management in a dental environment and particularly in the provision of conscious sedation. This paper presents a review on psychogenic non-epileptic seizures and discusses the considerations for assessment and dental treatment planning with or without conscious sedation. Finally, the authors present a case study of a patient who experienced PNES during dental treatment under conscious sedation.
Introduction
Psychogenic non-epileptic seizures (PNES) are conditions that may mimic epileptic seizures, convulsive movements, alterations in cognitive, sensory or motor functions, or altered behaviours that resemble epileptic seizures, but are not associated with abnormal electrical activity in the cortex.1,2 PNES are also referred to as functional seizures, dissociative seizures, non-epileptic seizures or psychogenic seizures and they are a common subtype of functional neurological disorder (FND).3 Other presentations of FND include functional limb weakness, tremors, dystonia, gait and cognitive disorder.3,4 Non-epileptic seizures may be precipitated by physiological causes such as hypoglycemia, other metabolic disorders, syncope and arrythmias;5,6 however, this paper does not discuss physiological causes for non-epileptic seizures under its remit.
Epidemiology and co-morbidities
PNES are more common than previously reported, although there is a lack of comprehensive epidemiological studies owing to the high incidence of misdiagnosis and delay in diagnosis.7,8 Some studies have reported the incidence for PNES to be around 3.1 - 4.9 in 100,000 population per year and prevalence of about 33 individuals in 100,000 population per year.9,10 Studies have shown that around 80% of individuals with PNES are females, although the gender discrepancy is less in other subtypes of FND.7 A vast majority of cases are diagnosed at 20-40 years, however, younger children and the elderly can also be affected.11 In a population-based study, Duncan et al. have discussed high rates of psychological morbidity and at least one other medically unexplained symptom other than PNES, suggesting increased overlap between PNES and other FND.10 A prospective one-year audit of people with PNES has shown higher emergency and non- emergency related healthcare demands including ambulance call outs, hospital admissions, MRIs and CT scans in the first six months of diagnosis.12
Adults with PNES have higher occurrence of co-morbidities which contribute to complex presentations, unpredictable treatment outcomes and a poorer prognosis.4,8 Commonly reported physical medical comorbidities include obesity, chronic fatigue syndrome, fibromyalgia, chronic pain, migraines and irritable bowel syndrome.13 Patients may also experience psychiatric symptoms of increased anxiety, depression, mood disorder and personality disorders.8 Furthermore, there tends to be a stronger association of PNES with post-traumatic stress disorder (PTSD) and estimates have suggested that around 75% of people with PNES have reported a prior traumatic experience such as sexual or physical abuse.14 Those with a prior history of sexual abuse are at risk of earlier PNES onset, more delay in diagnosis, increased severity of convulsions and emotional triggers.15
Epileptic seizures and PNES
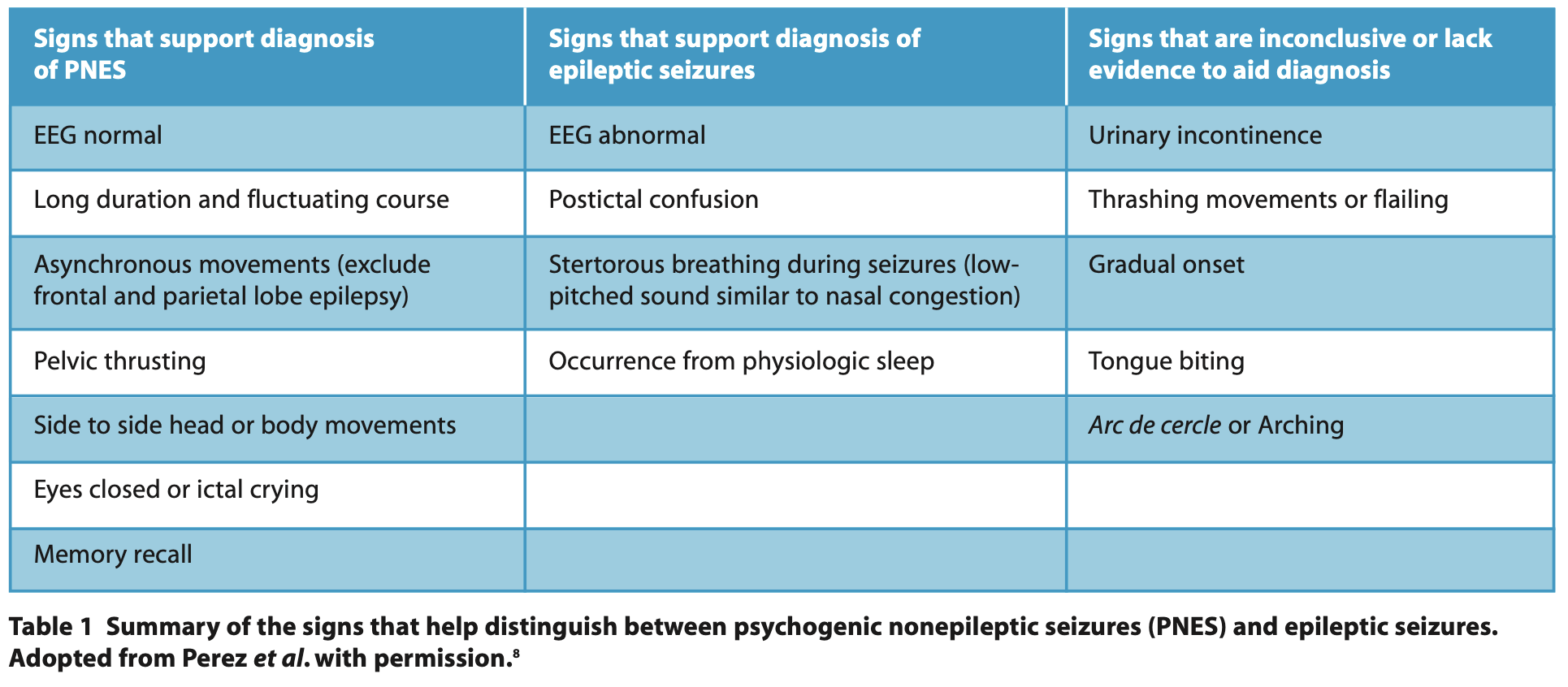
The distinction between epileptic seizure and PNES can be clinically challenging as there is no one pathognomonic sign that differentiates epileptic seizures and PNES.2,8 PNES diagnosis is favoured if there is a clinical presentation of events of longer duration (>10 min), asynchronous or side to side movements, ictal eye closure at onset or eye fluttering, ictal crying and post-ictal recall of information (Table 1).7,16 Recommendations from the International League Against Epilepsy suggest that the gold standard for diagnosis of PNES is a video recording of a typical event and electroencephalography (EEG) which can be used to record the absence of epileptiform activity on the EEG before, during and after a typical seizure with history consistent with PNES.8 However, this resource may not always be available.
To make diagnosis even more challenging, epileptic seizures and PNES can co-exist and may present in two forms: sequential, where treated epileptic seizures are followed by PNES; or simultaneous, where both PNES and epileptic seizures have been recorded within the same admission.17 The average frequency of epilepsy in patients with PNES is 22%, whereas 12% of people with known epilepsy may also have PNES.18 This patient group may also have poorer quality of life than those with epileptic seizures.3 Around 5-10% people attending outpatient epilepsy clinics and 20-40% of those receiving inpatient epilepsy care have PNES.1
Learning disability and PNES
Although the prevalence of PNES is relatively rare in the general population, 0.03%,9 it is reported to be up to 10% in people with learning disabilities.19,20 However, studies of this subgroup of PNES are limited.21 Evidence suggests that people with learning disabilities have greater prevalence of co-morbid epilepsy and history of negative life events such as trauma and stress which may precipitate or perpetuate PNES.20 They may also have a higher incidence of other psychiatric disorders such as anxiety, depression and PTSD.8 Furthermore, people with learning disabilities are more likely to experience a delay in diagnosis of PNES due to difficulties obtaining a coherent symptomatic history and difficulties measuring treatment outcomes because of limited data and higher risk of bias.20
Treatment
The treatment of PNES is based on an empathetic approach which acknowledges the ‘real’ nature of symptoms, as this condition is often considered as ‘pseudo-seizure’, leaving patients feeling stigmatised.22 Supportive therapy such as Cognitive Behavioural Therapy is the mainstay of treatment, which may not reduce frequency of seizures but improve overall health related quality of life outcome.23,24 This may be combined with antidepressants alongside therapy for additional psychiatric diagnosis such as PTSD, anxiety and depression, however, individuals may not become completely seizure-free.8,24 Anti-epileptic medications are not generally used for treatment unless there is a concomitant diagnosis of epilepsy.25
Dental considerations for conscious sedation in patients with PNES People with a seizure history are likely to have relatively poor oral health and increased history of trauma, leading to a high level of dental treatment.26,27 They are likely to need treatment in a community special care or hospital dental setting, especially if their seizures are unpredictable or challenging to control.26 PNES can occur in any environment but have been reported to occur in the peri-operative period with general anaesthesia (GA) and under local anaesthesia, for example, during dental extractions or restorations.28–30 PNES are often exacerbated by anxiety and stress.8 Whilst stress and anxiety reduction are likely to be useful in reducing seizures, there is a lack of evidence to support the effectiveness of either oral sedative premedication, or inhalation or intravenous sedation (IV) in reducing precipitation of PNES. Overall, there is a lack of evidence around recommendations for PNES management in the dental environment.26
Recommendations for assessment
Detailed seizure history
Seizure presentation, particularly if the patient already has a video recording, may provide insight into a ‘typical episode’. Clinicians should also obtain other key seizure details such as known triggers, duration of a typical episode, whether there is any loss of consciousness and duration of recovery in the post-ictal phase. It is also helpful to find out whether any physical trauma has ever been sustained due to seizures and the patient’s usual management of seizures. It is equally important to record whether there is a co-existing diagnosis of epilepsy alongside PNES and whether the seizures are sufficiently violent to require a hospital admission. The association of PNES with PTSD or past physical or sexual abuse, if known, may help us provide appropriate psychological support to the patient, although this is not always disclosed.
Past dental history
Seizure history concerning previous dental treatment can give vital information around known triggers within the clinical dental environment. Some case studies or anecdotal patient histories have reported exacerbation of symptoms of FND or seizures following administration of local anaesthesia, so obtaining these details will ensure safe delivery of care.28 Information on specific procedural anxieties will also help decision making around future care.
Social history
Dental practitioners should enquire about any people who usually support the patient for their dental appointment, including family members or carers, as this information will help dental teams to plan adequate support during appointments and safe discharge in the event of seizure.
Recommendations for treatment planning
Consider avoiding elective dental procedures for the first few months after the initial seizure until diagnostic investigations are completed and there have been no further hospital admissions.12 Liaise with the patient’s neurologist, psychiatrist or general practitioner as appropriate. Low dental anxiety and short dental procedures Short procedures may be managed well by the dental team who build good rapport with the patient. The use of behaviour management techniques and psychological support may be helpful. Application of topical anaesthesia and pain free administration of local anaesthetic may further reduce anxiety and oral premedication for anxiolysis may make travel to dental appointment easier.26
Moderate dental anxiety and mild to moderate invasive dental procedures For management of mild to moderate dental anxiety in people with seizures, a titrated mixture of nitrous oxide and oxygen inhalation sedation technique may be suitable.31 Inhalation sedation has a good safety record and the benefits of rapid onset and recovery. Inhalation sedation can be reversed quickly in an event of seizure, together with immediate administration of continuous oxygen. Multiple studies have shown it to be effective in reducing anxiety during dental procedures, especially for patients with mild-to-moderate dental anxiety.32 However, individual responses can vary and the efficacy can depend on factors such as level of anxiety, individual physiology, and the nature and extent of dental treatment planned.31 Inhalation sedation may not be appropriate for patients with high dental anxiety and those with more complex needs.26 High dental anxiety and invasive or prolonged dental procedures.
For people with seizures and high dental anxiety or those undergoing prolonged or invasive dental procedures, IV sedation with titrated midazolam can be effective.31 Midazolam itself is anxiolytic and has anticonvulsant properties, however, its use requires careful consideration of potential interactions with anti- epileptic medication. Antiepileptic medications such as carbamazepine, phenytoin, primidone and phenobarbital stimulate the activity of cytochrome P450 enzymes which may result in faster metabolism of midazolam and decreased blood levels.33,34 Furthermore, midazolam will not always prevent PNES, as anticonvulsants have no effect on PNES. If a patient is already on long term benzodiazepine therapy, then the sedative effect of midazolam sedation may be reduced due to drug tolerance. In addition, any use of flumazenil may reverse their existing benzodiazepine therapy.35 A detailed history will ensure optimal treatment planning and patient management in the event of a seizure, including when to consider hospital transfer. Clear communication with the patient, their carer and the dental team is essential.
Recommendations for emergency seizure management during PNES
In patients with known or suspected PNES, initial management is similar to that of an epileptic seizure.36
- Monitor airways, breathing and circulation
- Prevent patient injury
- Remain calm and reassuring
- Continue to monitor using the ABCDE approach37
- Consider use of NEWS score to assess suitability of time and environment for discharge. Ie based on NEWS score consider if discharge should be delayed (time) and additional monitoring needed and / or consider if the patient should be discharged home or advised regarding your local referral arrangements for out of hours admission (environment)
- Close liaison with carers / escort to ensure safe discharge.
Hospital transfer would be considered for those patients presenting with a seizure for the first time whose diagnosis is uncertain, or those with mixed epileptic and non-epileptic seizure patterns where differentiation between the two is challenging. Consider transfer to hospital for those with violent seizures causing injury to the patient or where there is an exacerbation of their FND symptoms needing further investigation or care. Unlike prolonged epileptic seizures, midazolam is not administered as a medical emergency drug to manage PNES but careful monitoring is essential.17
Case study
A 27-year-old female patient was referred to the community dental services by her general dental practitioner (GDP) owing to her history of seizures and high dental anxiety. The patient refused to undergo dental treatment with local anaesthesia alone. The patient’s past medical history included the following:
- Allergies to latex and kiwi fruit
- Well controlled asthma: managed by Clenil modulite 100 mcg/dose inhaler - 2 puffs twice daily, Salbutamol 100 mcg dose inhaler as needed
- Overactive bladder: Solifenacin 10 mg tablets once daily, D- mannose 500 mg 2 capsules daily
- Benign heart murmur: discharged from Cardiology
- Postural Orthostatic Tachycardia Syndrome (POTS)
- Autism
- Attention Deficit Hyperactivity Disorder (ADHD)
- Anxiety, panic attacks (triggers included hospital environments and dental treatment)
- Seizures linked to FND which can be triggered by stress and heightened anxiety. Seizures were reported as lasting a few seconds to minutes, with a tonic-clonic phase followed by loss of consciousness. The seizures usually occur in clusters and the patient usually has no memory of the event. Hospital transfer is not usually required as there has been no seizure related physical injury to date.
The patient had a significant dental phobia, particularly around the thought of injections of local anaesthesia and noise (scraping, drilling etc). Her only experience of operative treatment was for fixed upper and lower arch orthodontic appliances followed by the placement of permanent retainers. Her mother reported that the patient did not get on well with her GDP so did not go back for regular recalls for several years. Recently, her sensory issues had exacerbated her phobia to the extent that the patient found it difficult to brush her teeth regularly, resulting in a period of dental neglect. She consumed mainly squash and carbonated drinks, and habitually snacked on high cariogenic foods including biscuits. She used prescription sodium fluoride toothpaste and a manual toothbrush for oral hygiene once every two days. A social history revealed that the patient lived with both parents and was usually supported to dental appointments by her mother. She went to a local farm once a week where she enjoyed working with animals.
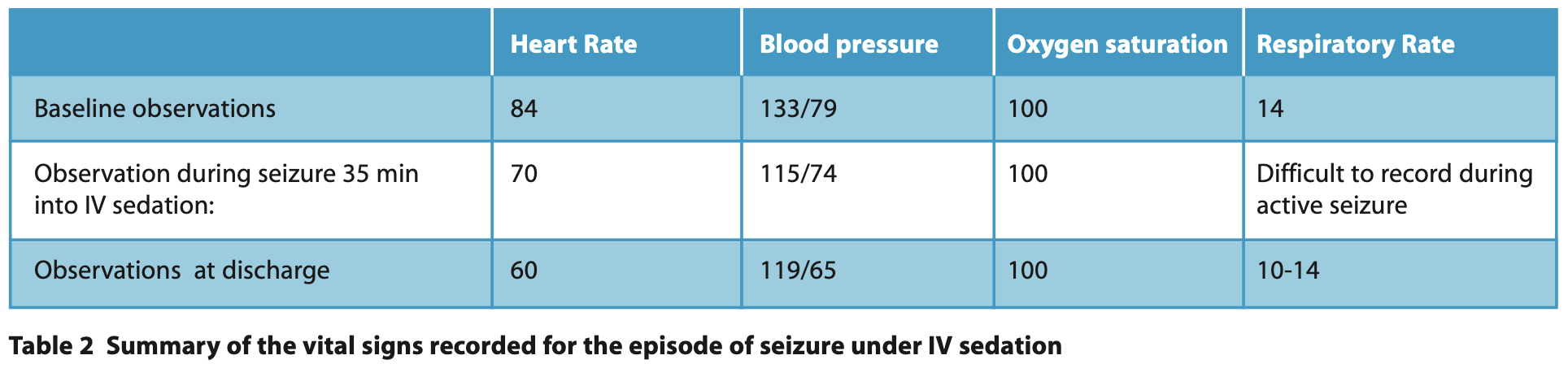
On examination, all four third molars were carious and partially erupted. She also had caries in all of her upper premolars, her upper anterior teeth as well as her left and right lower lateral incisors and canines. Her basic periodontal examination score was 1 or 2 in each sextant. She had marked gingivitis especially to her upper and lower labial surfaces from plaque accumulation and infrequent brushing. Caries in the anterior teeth was on interdental and buccal surfaces close to the permanent orthodontic retainers. At the initial assessment, the patient expressed a wish for sedation or GA for dental treatment as injection, noise and sensation of dental equipment was stress-provoking. Baseline observations were within normal range (Table 2). The options for treatment and pros and cons of each were discussed including inhalation sedation, IV sedation with midazolam and GA. The patient opted for IV sedation using midazolam, including oral premedication of 10mg Temazepam, taking one tablet the night before and one tablet on the morning of treatment, to help reduce pre-operative anxiety.
The patient’s first episode of dental treatment was managed under IV midazolam with prior oral temazepam premedication, as planned. Restorations were placed in UR2 UR3 UL3 UL4 and the patient’s vital signs remained normal throughout. The patient received a titrated dose of IV midazolam 1 mg/minute, to a total of 4 mg, and had a sedation score of 3 and operating condition score of 1. After about 40 minutes, the patient closed her eyes, became unresponsive, then had two episodes of tonic-clonic seizures lasting 10 seconds each with full recovery in between. Despite seizures, the patient was visibly relaxed during the entire sedation episode and was not distressed during or after seizures. As oxygen saturation remained at 100%, no supplemental oxygen was administered. During discharge, the patient declared that she felt ‘floppy’ in her legs and was monitored for an additional 30 minutes to allow better recovery. She used a wheelchair to get to her car and both her escort and the dental team supported the transfer to her car.
Due to her prolonged recovery post sedation, treatment modality options were discussed again with the patient and her parent. Inhalation sedation was discussed again as an alternative measure to help with anxiety which would also allow a quicker recovery. Subsequently, the patient agreed to try further restorations with inhalation sedation and she successfully completed three sessions of dental treatment with a titrated mixture of 35%- 40% nitrous oxide and oxygen. On the fourth visit, during an episode of simple restorations under inhalation sedation, the patient had more episodes of PNES, approximately 45 min into the sedation. At one point, she stopped responding, held her breath, closed her eyes, then started having tonic-clonic seizures; a total of 3 seizures within 10 minutes, but without any recovery in between on this occasion. The parent reported that this was the most usual seizure type for the patient. Once again, the patient was kept safe from injuries and monitored following the ABCDE approach. Fortunately, her vital signs and breathing remained normal, no intervention was needed and the patient recovered fully and was discharged safely home. This time she did not report any muscle or limb weakness after the episode. Her remaining treatment was continued with inhalation sedation and all restorative treatment was completed without further intra- operative seizure activity.
Conclusion
People with PNES are likely to have a varied presentation including complex medical or psychological co-morbidities. Guidance on management of these patients in a dental environment is very limited. An empathetic, patient-centred approach and careful history is essential in allowing the dental team to build rapport with their patients and discuss a seizure management plan. Most dental care may be safely provided in a primary care environment. Conscious sedation may prove to be a useful adjunct in managing underlying stress and dental anxiety which can trigger seizures in people with PNES. However, careful assessment is crucial to ascertain the most appropriate type of conscious sedation technique, together with the use of premedication to facilitate the safe delivery of care.
Bibliography
1. Alsaadi T M, Marquez A V. Psychogenic nonepileptic seizures. Am Fam Physician 2005; 72: 849–856.
2. Devinsky O, Gazzola D, LaFrance W C. Differentiating between nonepileptic and epileptic seizures. Nat Rev Neurol 2011; 7: 210–220.
3. Bennett K, Diamond C, Hoeritzauer I, Gardiner P, McWhirter L, Carson A et al. A practical review of functional neurological disorder (FND) for the general physician. Clinical Medicine 2021; 21: 28–36.
4. Hallett M, Aybek S, Dworetzky B A, McWhirter L, Staab J P, Stone J. Functional neurological disorder: new subtypes and shared mechanisms. Lancet Neurol 2022; 21: 537–550.
5. Josephson C B, Rahey S, Sadler R M. Neurocardiogenic Syncope: Frequency and Consequences of its Misdiagnosis as Epilepsy. Canadian Journal of Neurological Sciences / Journal Canadien des Sciences Neurologiques 2007; 34: 221–224.
6. Bosak M, Sowa-Staszczak A, Słowik A. Insulinoma mimicking psychogenic non- epileptic seizures in a patient with refractory epilepsy. Pol Arch Intern Med 2019; 129: 7–8.
7. Aybek S, Perez D L. Diagnosis and management of functional neurological disorder. BMJ 2022; 376.
8. Perez DL, LaFrance W C. Nonepileptic seizures: an updated review. CNS Spectr 2016; 21: 239–46.
9. Asadi-Pooya A A. Incidence and prevalence of psychogenic nonepileptic seizures (functional seizures): a systematic review and an analytical study. Int J Neurosci 2023; 133: 598–603.
10. Duncan R, Razvi S, Mulhern S. Newly presenting psychogenic nonepileptic seizures: incidence, population characteristics, and early outcome from a prospective audit of a first seizure clinic. Epilepsy Behav 2011; 20: 308–11.
11. Duncan R, Oto M. Predictors of antecedent factors in psychogenic nonepileptic attacks: multivariate analysis. Neurology 2008; 71: 1000–5.
12. Razvi S, Mulhern S, Duncan R. Newly diagnosed psychogenic nonepileptic seizures: health care demand prior to and following diagnosis at a first seizure clinic. Epilepsy Behav 2012; 23: 7–9.
13. Dixit R, Popescu A, Bagić A, Ghearing G, Hendrickson R. Medical comorbidities in patients with psychogenic nonepileptic spells (PNES) referred for video-EEG monitoring. Epilepsy Behav 2013; 28: 137–40.
14. Myers L, Perrine K, Lancman M, Fleming M, Lancman M. Psychological trauma in patients with psychogenic nonepileptic seizures: Trauma characteristics and those who develop PTSD. Epilepsy & Behavior 2013; 28: 121–126.
15. Selkirk M, Duncan R, Oto M, Pelosi A. Clinical differences between patients with nonepileptic seizures who report antecedent sexual abuse and those who do not. Epilepsia 2008; 49: 1446–1450.
16. LaFrance W C, Baker G A, Duncan R, Goldstein L H, Reuber M. Minimum requirements for the diagnosis of psychogenic nonepileptic seizures: a staged approach: a report from the International League Against Epilepsy Nonepileptic Seizures Task Force. Epilepsia 2013; 54: 2005–18.
17. El-Naggar H, Moloney P, Widdess-Walsh P, Kilbride R, Delanty N, Mullins G. Simultaneous occurrence of nonepileptic and epileptic seizures during a single period of in-patient video-electroencephalographic monitoring. Epilepsia Open 2017; 2: 467–471.
18. Kutlubaev M A, Xu Y, Hackett M L, Stone J. Dual diagnosis of epilepsy and psychogenic nonepileptic seizures: Systematic review and meta-analysis of frequency, correlates, and outcomes. Epilepsy Behav 2018; 89: 70–78.
19. Duncan R, Oto M. Psychogenic nonepileptic seizures in patients with learning disability: comparison with patients with no learning disability. Epilepsy Behav 2008; 12: 183–6.
20. Rawlings G H, Novakova B, Beail N, Reuber M. What do we know about non- epileptic seizures in adults with intellectual disability: A narrative review. Seizure 2021; 91: 437–446.
21. van Ool J S, Haenen AI, Snoeijen-Schouwenaars F M, Aldenkamp A P, Hendriksen J G M, Schelhaas H J et al. Psychogenic nonepileptic seizures in adults with epilepsy and intellectual disability: A neglected area. Seizure 2018; 59: 67–71.
22. Tilahun B B S, Bautista J F. Psychogenic nonepileptic seizure: An empathetic, practical approach. Cleve Clin J Med 2022; 89: 252–259.
23. Hopp J L. Nonepileptic Episodic Events. Continuum (Minneap Minn) 2019; 25: 492–507.
24. Goldstein L H, Robinson E J, Mellers J D C, Stone J, Carson A, Reuber M et al. Cognitive behavioural therapy for adults with dissociative seizures (CODES): a pragmatic, multicentre, randomised controlled trial. Lancet Psychiatry 2020; 7: 491–505.
25. LaFrance W C, Baird G L, Barry J J, Blum A S, Frank Webb A, Keitner GI et al. Multicenter pilot treatment trial for psychogenic nonepileptic seizures: a randomized clinical trial. JAMA Psychiatry 2014; 71: 997–1005.
26. Ransford N, Soryal I, McCorry D, Sander J W, Duncan F, Huggins N. Specialist management of routine dental procedures in adults with refractory epilepsy. Br Dent J 2014; 216: 403–7.
27. Károlyházy K, Kovács E, Kivovics P, Fejérdy P, Arányi Z. Dental Status and Oral Health of Patients with Epilepsy: An Epidemiologic Study. Epilepsia 2003; 44: 1103–1108.
28. Goss A. Functional neurologic disorder as a rare complication of dental local anaesthetics: two contrasting cases. Br Dent J 2024; 236: 97–99.
29. Dusara K, Davies S, Lee Y. Functional neurological disorder: a review. Br Dent J 2023; 235: 112–116.
30. Reuber M, Enright S M, Goulding P J. Postoperative pseudostatus Not everything that shakes is epilepsy. Anaesthesia 2000; 55: 74–78.
31. Stanley F Malamed. Sedation A guide to patient management. 6th ed. Elsevier, 2017.
32. Hierons R J, Dorman M L, Wilson K, Averley P, Girdler N. Investigation of inhalational conscious sedation as a tool for reducing anxiety in adults undergoing exodontia. Br Dent J 2012; 213: E9–E9.
33. Hayashi T, Higuchi H, Tomoyasu Y, Ishii-Maruhama M, Maeda S, Miyawaki T. Effect of carbamazepine or phenytoin therapy on blood level of intravenously administered midazolam: a prospective cohort study. J Anesth 2016; 30: 166–169.
34. Penninga E I, Graudal N, Ladekarl M B, Jürgens G. Adverse Events Associated with Flumazenil Treatment for the Management of Suspected Benzodiazepine Intoxication – A Systematic Review with Meta-Analyses of Randomised Trials. Basic Clin Pharmacol Toxicol 2016; 118: 37–44.
35. epilepsysociety.org.uk. https://epilepsysociety.org.uk/about-epilepsy/what-epilepsy/non-epileptic-functional-dissociative-seizures accessed 18 Sep2024).
36. Resuscitation council UK. Resuscitation Council UK The ABCDE Approach. October 2015. https://www.resus.org.uk/library/abcde-approach (accessed 18 Sep 2024).