Please click on the tables and figures to enlarge
Clinical audit on the quality of written consent for inhalation sedation
R. Corden*1 NEBDN National Diploma Dental Nursing and NEBDN Award in Intravenous Sedation Nursing
1Dental Nurse, Barnstaple NHS Dental Access Centre, Barnstaple Health Centre, Vicarage Street, Barnstaple, Devon, EX32 7BH
*Correspondence to: Rebecca Corden
Email: r.corden@nhs.net
Corden R. Clinical audit on the quality of written consent for inhalation sedation SAAD Dig. 2025: 41(I): 62-65
Abstract
Valid written consent is mandatory for all dental treatment that is carried out under conscious sedation. Clinical teams have a duty to evidence that valid consent was obtained via appropriate discussion with patients or their legal guardians. Good quality clinical records are vital to show that appropriate discussions have been undertaken and to aid in future clarity should queries arise from patients or their legal guardians. This loop-closure audit focuses on whether written consent forms were correctly and accurately completed prior to treatment being carried out under inhalation sedation within salaried dental services at Royal Devon University Healthcare NHS Foundation Trust and covers both Exeter Dental Access Centre and Barnstaple Dental Access Centre. It shows that there was a substantial improvement in accurately completed written consent forms, after an action plan was created and discussion at the Joint Service Meeting, from 43% to 90% between the initial audit and re-audit.
Key learning points
- To measure the accuracy of written consent for conscious sedation technique using inhalation sedation
- To acknowledge the importance of recording informed consent as per GDC’s standards
- To identify key elements of consent from the record keeping point of view.
Introduction
The General Dental Council’s (GDC) ‘Standards for the Dental Team’ sets out the expectation around valid consent for all dental treatment. It states that valid written consent must be obtained and recorded for all patients treated under conscious sedation and/or general anaesthesia (Standards and their guidance 3.1.6).1 This document also states that sufficient details must be discussed during this process with enough time given for the patient to reach their own decision.
Guidance from dentolegal indemnity providers mention that enough information must be discussed with the patient or their legal guardian, and that the patient has a right to all the relevant information. The consent should be voluntary and informed and accurate written records must be kept of these discussions with the patient at the practice where conscious sedation is provided.2
Holden et al., have published a practical guide to gaining and recording consent for the dental team and the importance of this in avoiding complaints, litigation and improving patient autonomy.3
Finally, the Faculty of General Dental Practitioners (GDP) have set standards in their publication, ‘Clinical Exam and Record-keeping’, which include the need for valid written consent before treatment is undertaken under conscious sedation.4
This audit assessed whether correctly and accurately completed written consent is available for patients treated under conscious sedation using standard inhalation sedation technique at Exeter and Barnstaple Dental Access Centres. The primary benefit is to the patient, as any disparities or misunderstandings can be referred back to the written consent, by the patient or the dentist, on the fully completed consent form.
Aims
To measure the current standard of consent, regarding the provision of inhalation sedation, against the GDC’s Standards Principle three, with the aim of identifying any shortcomings, subsequent learning, and to action any necessary changes to pursue constant improvement.
Objectives
As per the GDC Standards Principle three, it was decided that all patients treated under conscious sedation should have written consent recorded in their clinical records, which should be fully and correctly completed with details of the patient and consenting dentist, details of the treatment proposed and use no abbreviations, as per the Trust’s consent forms used in the local department.
Method
This was a loop closure audit. The first cycle sample included 21 consecutive patients, both children and adults, treated under conscious sedation using inhalation sedation at both Exeter Dental Access Centre and Barnstaple Dental Access Centre in April 2023. Data was collected retrospectively by Rebecca Corden (dental nurse at Barnstaple Dental Access Centre) and Hiral Patel (senior dentist at Exeter and Barnstaple Dental Access Centres).
Written consent paperwork was examined closely and data were collected on the missing information identified:
- Demographics: patient details, parent details (if appropriate), dentist details, age, date of birth, NHS number, signatures from patient or parent / guardian and clinician
- Treatment details: Details of all proposed treatment correctly and accurately completed without abbreviations and including notation of teeth to be treated, risks and benefits discussion recorded in appropriate sections.
R4 dental software was checked to ascertain whether written consent was verbally confirmed on the day with the patient or parent / guardian.
Re-audit included 20 consecutive patients (10 from each of the Dental Access Centres) between November and December 2023. Rebecca Corden and Hiral Patel undertook data collection at each of the above sites and analysed it as above.
Results
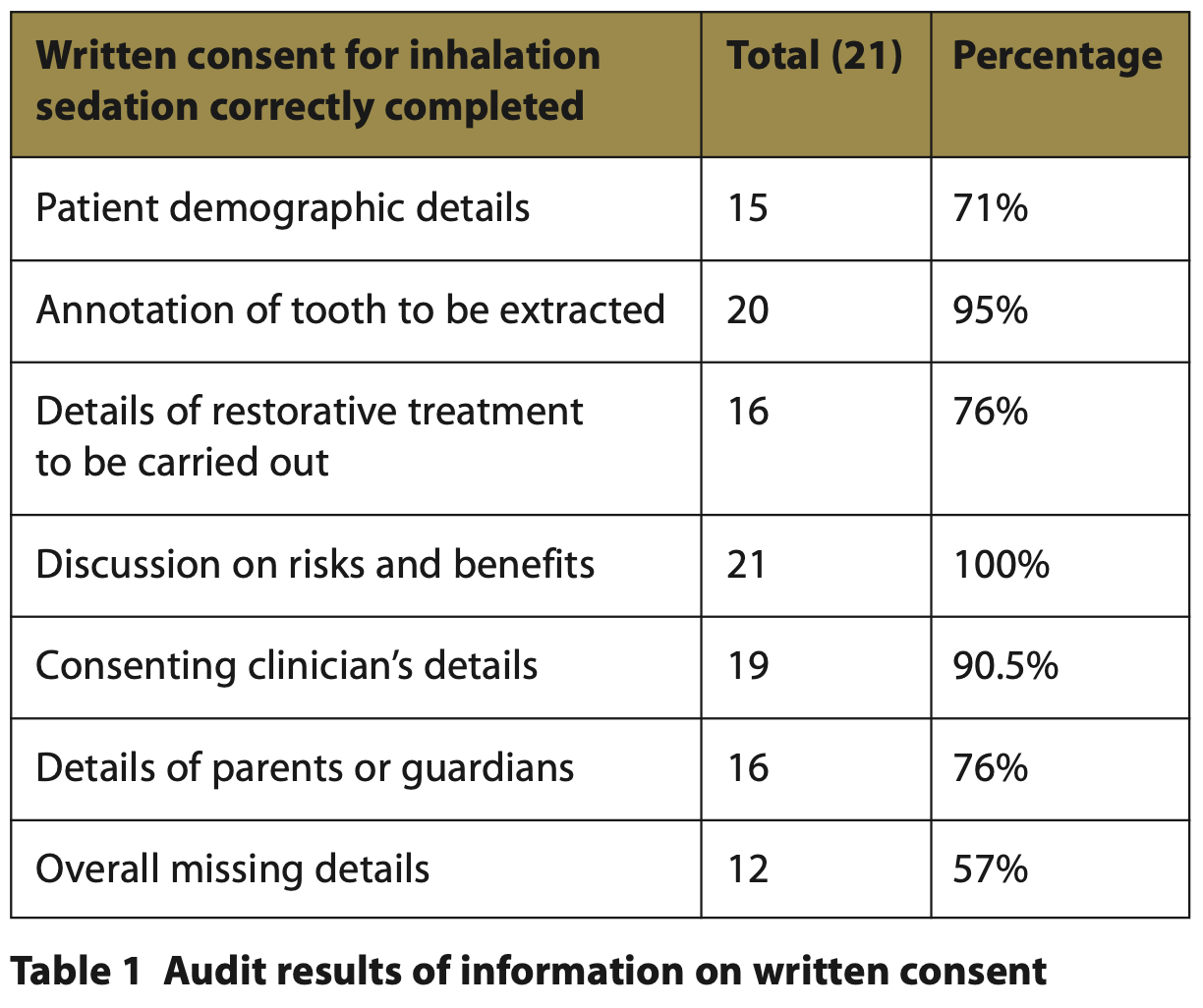
For the 21 consecutive patients who were audited in April 2023, undergoing inhalation sedation:
One hundred percent of patients included in the audit had written consent available. These are from 1 or 2 consent forms and are kept in the patient files.
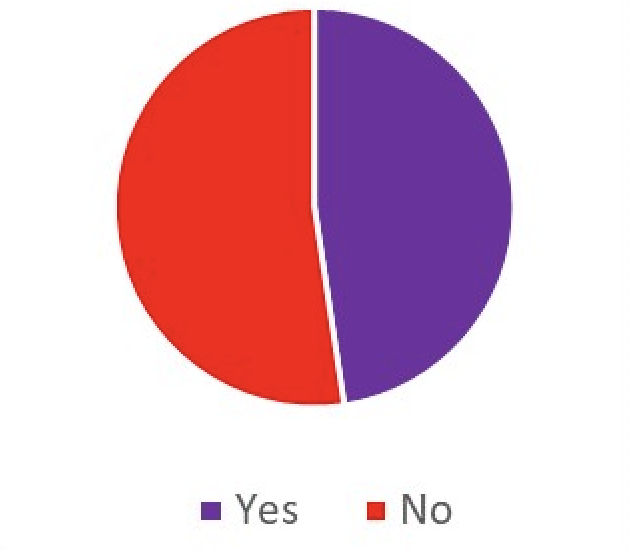
Forty three percent (9/21) of patients had consent forms correctly and accurately completed with no omissions of treatment details or demographics. Fifty three percent (12/21) of patients had missing information in the written consent form.
One hundred percent of patients included in this audit had a note on R4 record that consent was confirmed on the day with the patient or parent / guardian. R4 is our system where all patient notes are kept, these notes are made contemporaneously and accurately at the time of the appointment.
One hundred percent of patients had consent forms that had fully listed the risks and benefits of the treatment to be completed.
Fig. 1 Consent forms correctly and fully filled out
The omissions identified in written consent forms included demographics such as clinicians’ titles, patient NHS number, patient gender, the date the consent was signed by the patient or parent / guardian and names of parent / guardian where appropriate.
Some forms also had omissions of treatment details. Examples: treatment proposed would be filled with generic information such as ‘fillings’ without notations of which teeth were to be filled.
6/21 (29%) of the written consent forms were filled without the NHS numbers.
5/21 (24%) of the written consent forms were filled without the parent’s / guardian’s details (their signature was present but no names or date of signature).
1/21 (5%) of patients had a missing annotation of the tooth to be extracted.
5/21 (24%) of the treatment details for the fillings in the teeth were missing, such as the annotations of the teeth to be filled.
All written consent forms had completed the risks and benefits sections.
Discussion
The results of this audit show that written consent was always obtained for all persons with capacity or from their parents / legal guardians, undergoing dental treatment with conscious sedation.
However, the quality of record keeping around written consent could be improved in at least half of the records identified in this audit. The areas of improvement identified in at least a quarter of records assessed in this audit were inadequate demographic details of both patients and clinicians. More significantly, details of treatment proposed with the individual tooth annotation was also omitted in just under a third of the records assessed.
The missing demographic details can lead to problems with patient identification and parts of records can potentially be misfiled or go missing. (Written consent at the time of the audit was still in paper records with the rest of the dental record being on the R4 system). In areas where a parent / guardian has signed a record but not placed their name under the signature, difficulties may arise in identifying that individual at a later date. The missing details of the treatment may pose a more significant problem around patient information - a patient may be able to claim that they were not given full information of the proposed treatment under sedation, rendering their consent invalid.
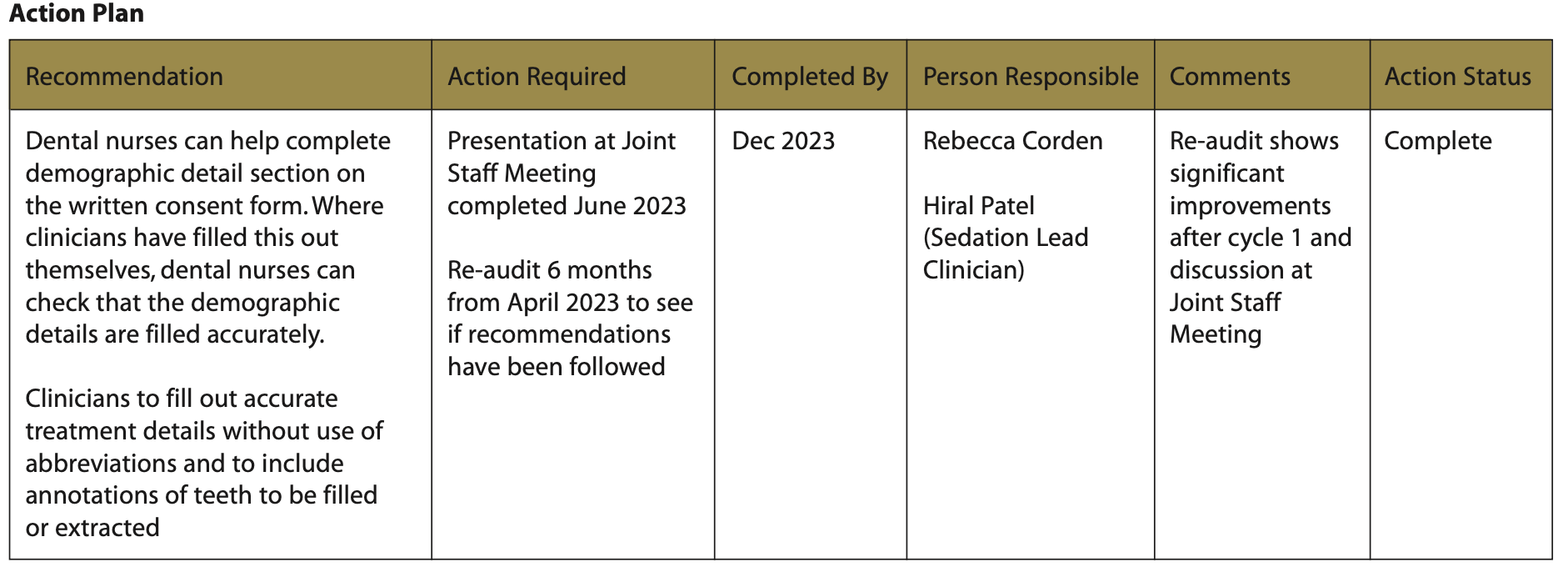
Recommendation
- Presentation at Joint Staff Meeting to ensure all sedation staff are aware of the results of the audit and the recommended changes going forward
- Dental nurses can help complete the demographic detail section on the written consent form. Where clinicians have filled this out themselves, dental nurses can check that the demographic details are filled accurately
- Clinicians to fill out accurate treatment details without the use of abbreviations and to include annotations of the teeth to be filled or extracted
- Re-audit to check that above interventions have been successful.
This audit was presented at the local Joint Staff Meeting attended by the clinical team (clinicians and nurses) and the above findings were discussed (Monday, 5 June 2023).
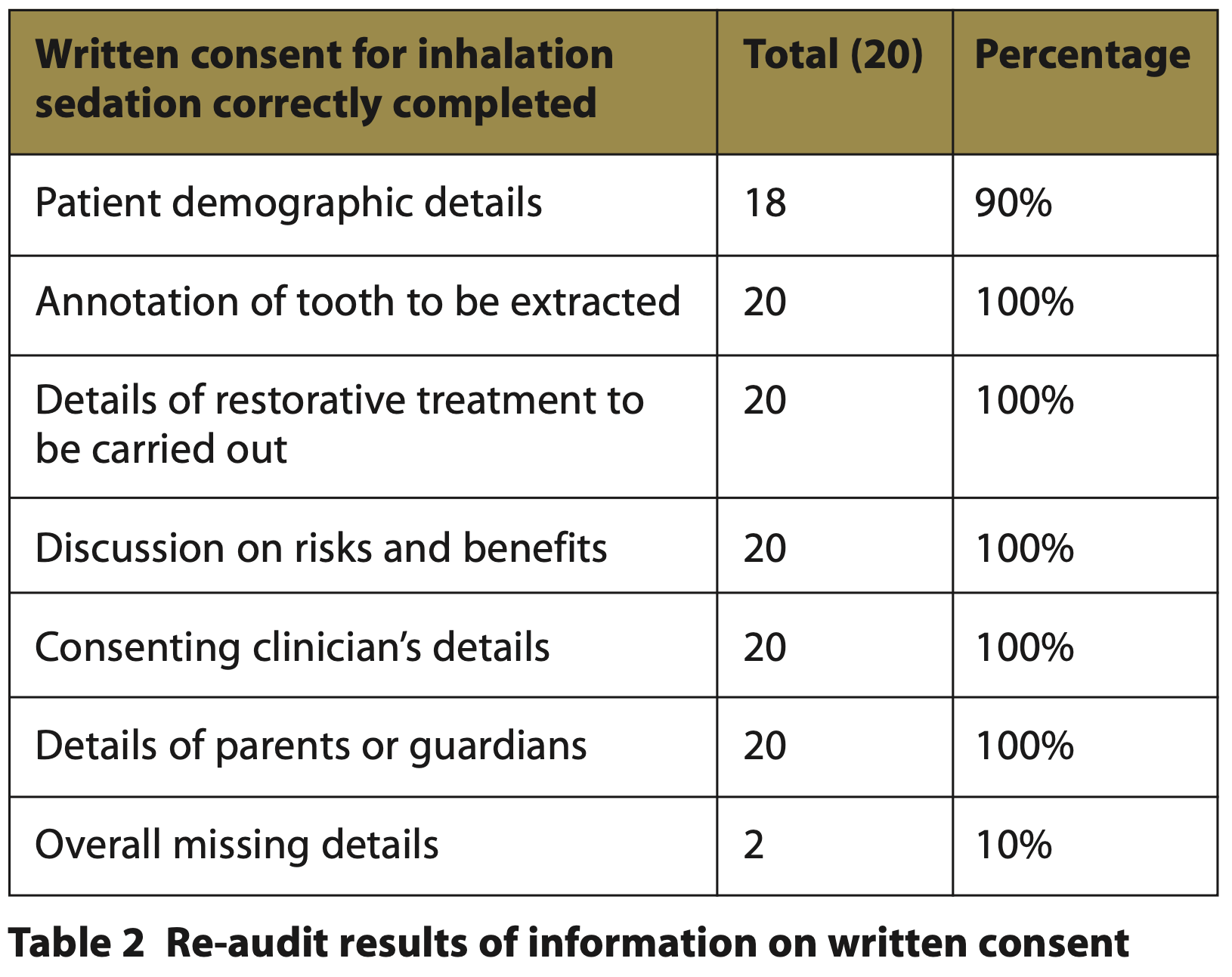
Re-audit findings
The re-audit was conducted between November 2023 and December 2023, six months after the initial audit to identify that the changes implemented in the action plan were effective. Patients that were included in the re-audit were from Barnstaple Dental Access Centre and Exeter Dental Access Centre.
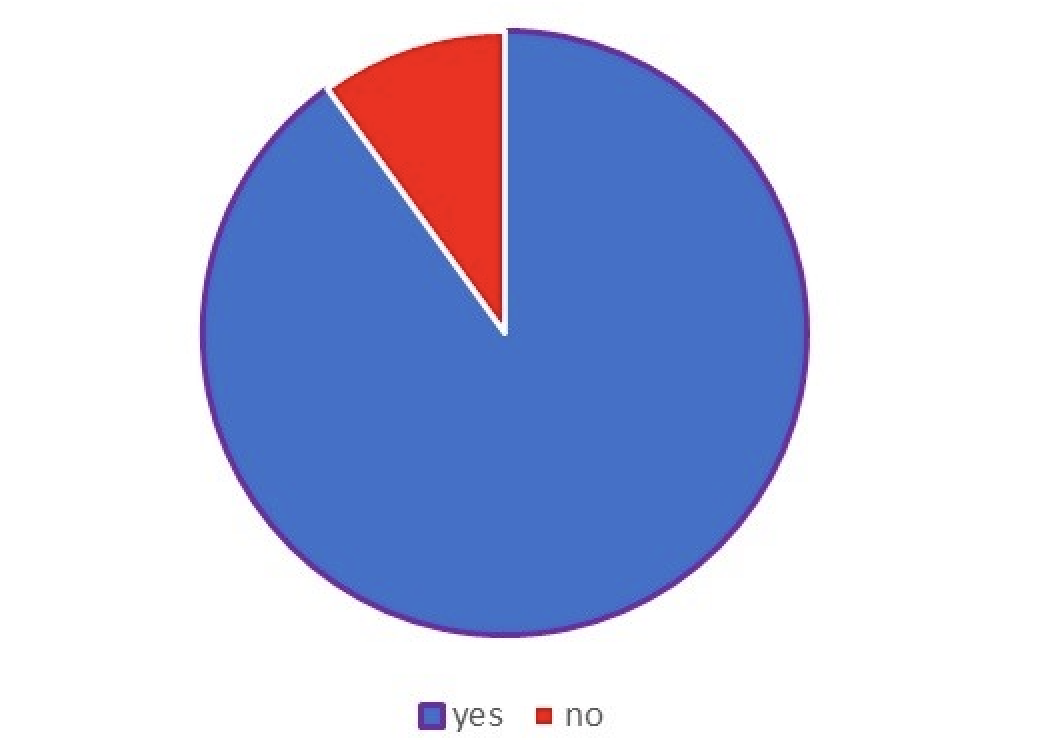
Fig. 2 Re-audit consent forms correctly and fully completed
The results of the re-audit show there has been a significant improvement in record keeping after discussion at the Joint Service Meeting.
All 20 patients (100%) included in this audit had completed written consent documentation in their records.
One hundred percent of patients had correct, accurate patient details, parent / guardian details where appropriate, and clinicians’ details.
One hundred percent of patient consent forms had accurate treatment details including annotations of the teeth to be treated.
Ninety percent (18/20) of patients had accurately completed consent forms with no omissions.
Ten percent (2/20) of patients had a small omission of NHS number on the consent forms with the rest of the details correctly completed.
In both the audit and re-audit, the full risks and benefits of the treatments that were to be carried out were recorded on the written consent forms.
Limitations of the study:
- No data was collected on the mental capacity assessment or best interest decision making for patients who were deemed to lack capacity to consent
- No data was collected on other forms of sedation such as IV sedation (as the majority of patients receiving treatment under IV sedation during the time were also lacking capacity to consent)
- Written consent is not always an accurate representation of the discussion of consent with the patient. This study is a retrospective audit and is not able to comment on the clinical discussion with patients in the process of valid consent. A peer review session may be able to provide better insight into the quality of discussion around consent. However, conducting such audits leads to increased awareness in the team and better record keeping.
Conclusion
Re-audit of this project shows significant improvement in the documentation of written consent for patients treated under inhalation sedation. Overall, the records had no omissions of treatment proposed, clinicians’ details, dates and signatures. A small omission of the patient’s NHS number was identified in two records and will be discussed at the next Joint Staff Meeting.
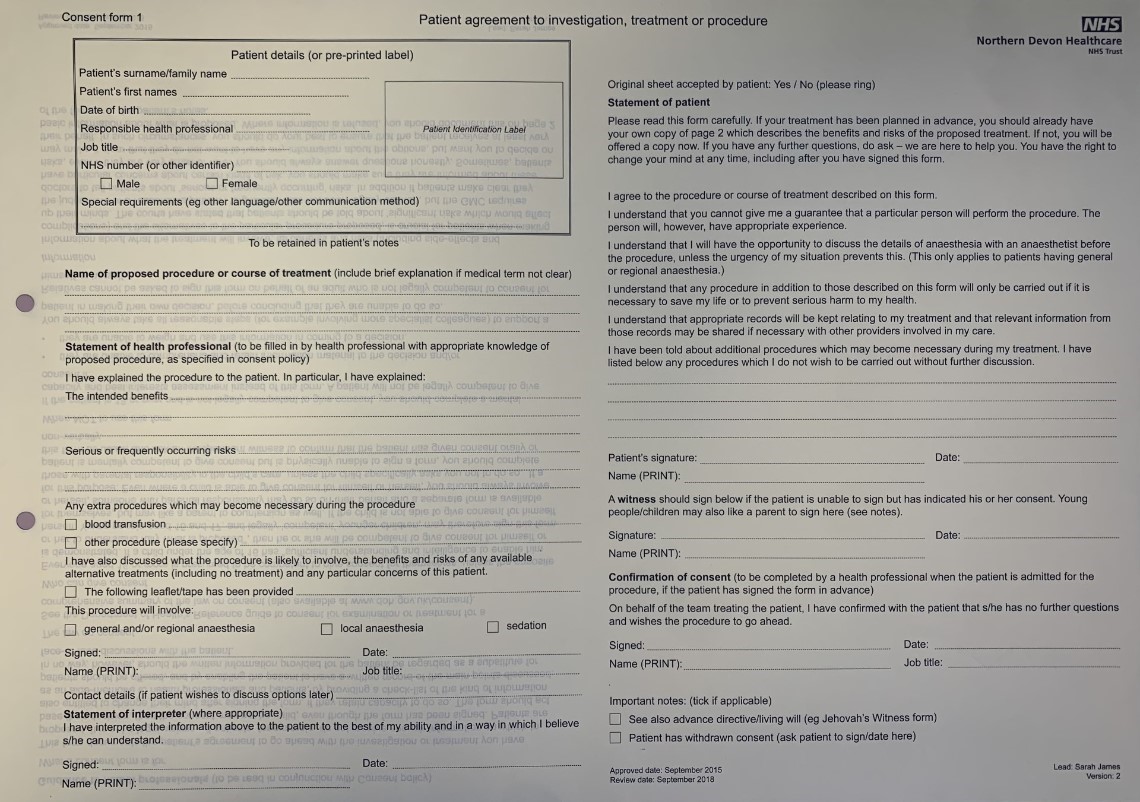
Fig. 3 Consent form sample: adult
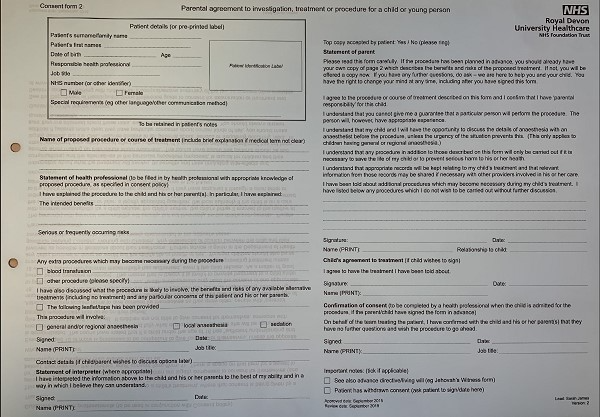
Fig. 4 Consent form sample: child
References
1. General Dental Council. Standards for the dental team. 2013. Online information available at: https://standards.gdc-uk.org/ (accessed Jan 2024)
2. Dental Defence Union. Guide to consent to dental treatment. 2022. Online information available at: https://www.theddu.com/guidance-and-advice/guides/quick-guide-to-consent (accessed Jan 2024)
3. Holden A C. Gaining and recording consent: a practical guide for the dental team. Prim Dent J. 2015; 4: 54-9. DOI: 10.1177/205016841500400119
4. Faculty of General Dental Practice (UK). Clinical Examination & Record-Keeping: Good Practice Guidelines. 2nd ed. London: FGDP(UK); 2009.