
Please click on the tables and figures to enlarge
Dental management under general anaesthesia of an adult patient with complex mental health considerations and learning disability
A. Dhanji*1(BDS, MFDS, DSCD, MSCD)
J. Perry2 (BDS, PG Dip Cons Sed, MSCD)
1Specialist in Special Care Dentistry, Birmingham Community Healthcare Trust, Birmingham Dental Hospital, 5 Mill Pool Way, Birmingham, B5 7EG
2Consultant in Special Care Dentistry, Birmingham Community Healthcare Trust, Birmingham Dental Hospital, 5 Mill Pool Way, Birmingham, B5 7EG
*Correspondence to: Dr Ayman Dhanji
Email: ayman.dhanji@nhs.net
Dhanji A, Perry J. Dental management under general anaesthesia of an adult patient with complex mental health considerations and learning disability. SAAD Dig. 2025: 41(I): 36-39
Case Summary
A 24-year-old male from an inpatient mental health secure hospital was referred to the Special Care Community Dental Services department with dental pain. Initial assessment confirmed a high dental need, complex medical and social history. This included Klinefelter syndrome, learning disability with associated behaviours of distress, autism, attention deficient hyperactive disorder (ADHD), obesity and high body mass index (BMI), asthma, type II diabetes mellitus, hearing impairment, plus severe needle phobia. Following evaluation of mental capacity status and risk assessment (medical, social and dental), reasonable adjustments were made to carry out comprehensive dental treatment under general anaesthetic (GA). This case demonstrates the importance of preparation and a multi-disciplinary team risk management approach to achieve a successful outcome and positive experience for this patient.
Patient details
- Gender: Male
- Age at start of treatment: 24
Pre-treatment asessment
This patient was referred from an inpatient mental health secure unit (IMHSU) which specialises in adults with learning disability, he had a severe needle phobia and had not accepted dental treatment since childhood. There was a background of behaviours which challenge secondary to his mental health, learning disability and autism. On initial assessment, he presented with dental pain, uncontrolled medical co-morbidities and a recent admission in hospital due to COVID-19 pneumonia. He attended with 3:1 escort and Ministry of Justice leave for medical interventions.
History of presenting patient’s complaints
Dental pain in his lower left quadrant which was impacting his eating habits. There was no history of swelling.
Relevant medical history
Klinefelter Syndrome (extra X chromosome), moderate learning disability, autism, ADHD, type II diabetes mellitus, asthma, class 3 obesity (BMI: 45) and hearing impairment.
Dental history
Inhalation sedation for dental treatment in childhood; thereafter there had been no dental intervention. His brushing habits were inconsistent and highly cariogenic diet.
Social history
Resides in IMHSU, 3-1 escort, minimal verbal communication. Uses vapes, nil alcohol.
Clinical examination
Extra-oral findings
No abnormalities detected (NAD)
Intra-oral findings
Soft tissues:
Buccal draining sinus adjacent to LL6
Hard tissues:
- Retained roots: LR7, LL6, LL7
- Caries: URC (distal), UL2 (mesial/ distal), LLE (mesial/distal),
- UL6 (occlusal)
- Poor oral hygiene
- UR3 palpable buccally, unerupted intra-orally
- BPE: not tolerated due to anxiety around probing
General radiographic examination
The patient initially refused radiographic examination, but following explanation and encouragement from his support workers agreed to an orthopantogram (OPG). He did not tolerate intra-oral radiographs.
Radiographs taken Monday, 7 February 2022
Justification: OPG was taken to identify caries status, periapical pathology and assess location of ectopic UR3
Grade: diagnostically acceptable
Findings:
- Periapical pathology associated with: LR7, LLE67
- UR3 present, unable to assess position without parallax
- UR7O, URC (distal), UL2M/D, LR6O radiolucencies consistent with caries
- Minimal generalised horizontal alveolar bone loss
Radiographs taken Thursday, 25 May 2023
Justification: OPG was taken to assess progression of dental disease and support treatment planning under GA
Grade: diagnostically acceptable
Findings:
- Retained roots: UR7C, LLE67, LR7
- Periapical pathology associated with: UR7C, LLE67, LR7
- UR3 present
- UR6O, UR5M/D, UR4M/D, UL1D, UL2M/D, UL6O, LL8O, LR4D, LR6O radiolucencies consistent with caries
- Minimal generalised horizontal alveolar bone loss
Diagnostic summary
Following clinical examination under general anaesthesia and radiographic examination, the following dental diagnoses were made:
- Retained roots with periapical periodontitis: UR7C, LLE67, LR7
- Unrestorable caries: UL2, LL8
- Restorable caries: UR6O, UR5M/D, UR4M/D, UL1D, UL6O, LR4D, LR6O
- Retained deciduous teeth: URC, LLE
- Ectopic unerupted UR3
- Generalised plaque induced gingivitis
Caries risk: high Periodontal risk: high Oral cancer risk: moderate
Aims and objectives of treatment
- To provide comprehensive dental treatment with a treatment modality suitable for the patient’s medical, social and dental risk factors
- To remove poor prognosis teeth and stabilise dentition to remove sources of pain and infection
- To provide a successful outcome and positive patient experience to support future medical and dental interventions.
Treatment plan
Comprehensive dental treatment was undertaken under GA at a medically supported tertiary hospital setting including:
- Full mouth professional mechanical plaque removal
- Extractions: UR7C, UL2, LL876E, LR78
- Restorations: UR6O, UR5M/D, UR4M/D, UL1D, UL6O, LR4D, LR6O
Treatment undertaken
- 7 February 2022: Emergency examination – at this appointment, multi-quadrant treatment need was established. Due to the patient’s mental health challenges and dental anxiety (MDAS – 25), dental treatment under local anaesthetic and inhalation sedation was refused and analgesic advice provided. Baseline measures were undertaken for intravenous sedation assessment: blood pressure- 124/74mmHg , SpO2 - 94%, BMI: 45 with central obesity, neck circumference- >40cm and possibility of obstructive sleep apnoea (STOPBANG 6: high risk).1 Following initial discussion, it was decided that anaesthetic opinion would be sought regarding suitability for intravenous sedation or GA and a conversation with the patient’s mother regarding his previous dental experiences.
- 11 April 2022 / 12 September 2022 / 20 February 2023: three planned visits to community dental services – patient did not attend (DNA). Following a series of DNA visits, the IMHSU were contacted for a case discussion with those involved in the patient’s medical care and family members to discuss how to support the patient’s attendance to dental visits as there was refusal to attend due to a combination of unstable mental health and dental anxiety. Anaesthetic opinion advised against any form of sedation outside of a medically supported setting and advocated for GA to safely carry out the patient’s dental care.
- 27 February 2023: Case discussion over Microsoft Teams
 Fig 1. Parties involved in case discussion
Fig 1. Parties involved in case discussion
A plan was made to visit the patient in his own environment at the IMHSU as a domiciliary visit with the following objectives:
- To increase rapport and trust in the dental professionals
- To assess his mental capacity
- To briefly discuss options for treatment
- To share the anaesthetic opinion.
- 24 April 2023: Domiciliary visit – two clinicians attended the IMHSU and spoke with the patient to assess his mental capacity. It was determined that he did not have capacity to make decisions regarding his dental and anaesthetic options for care as he was unable to understand risks, benefits and limitations of each option. Clinical photographs were taken of the patient’s airway to support remote anaesthetic assessment which displayed large neck circumference and short neck. Arrangements made for a follow-up visit for radiographs and best interests meeting (BIM).
- 25 May 2023: Community clinic visit for OPG radiograph which showed progression of dental disease since initial visit
- 31 July 2023: BIM over Microsoft Teams with all parties involved in the patient’s care to discuss treatment options – it was determined that comprehensive dental care under GA was the least restrictive and safest approach in line with the principles of the Mental Capacity Act 2005.2 The risks and benefits of the treatment were discussed. The patient journey (peri-operative, intra-operative and post-operative) was discussed with the appropriate reasonable adjustments to ensure safety of the patient and staff throughout. A clinical holding risk assessment was completed.3 Written consent was completed to evidence the treatment plan in the patient’s best interests.

Fig 2. Parties involved in best interests meeting
vii. 9 August 2023: Comprehensive dental treatment completed under GA as per above plan including blood tests as advised by the patient’s medical team.
viii. 12 August 2023: Telephone review after treatment where it was reported he was recovering well.
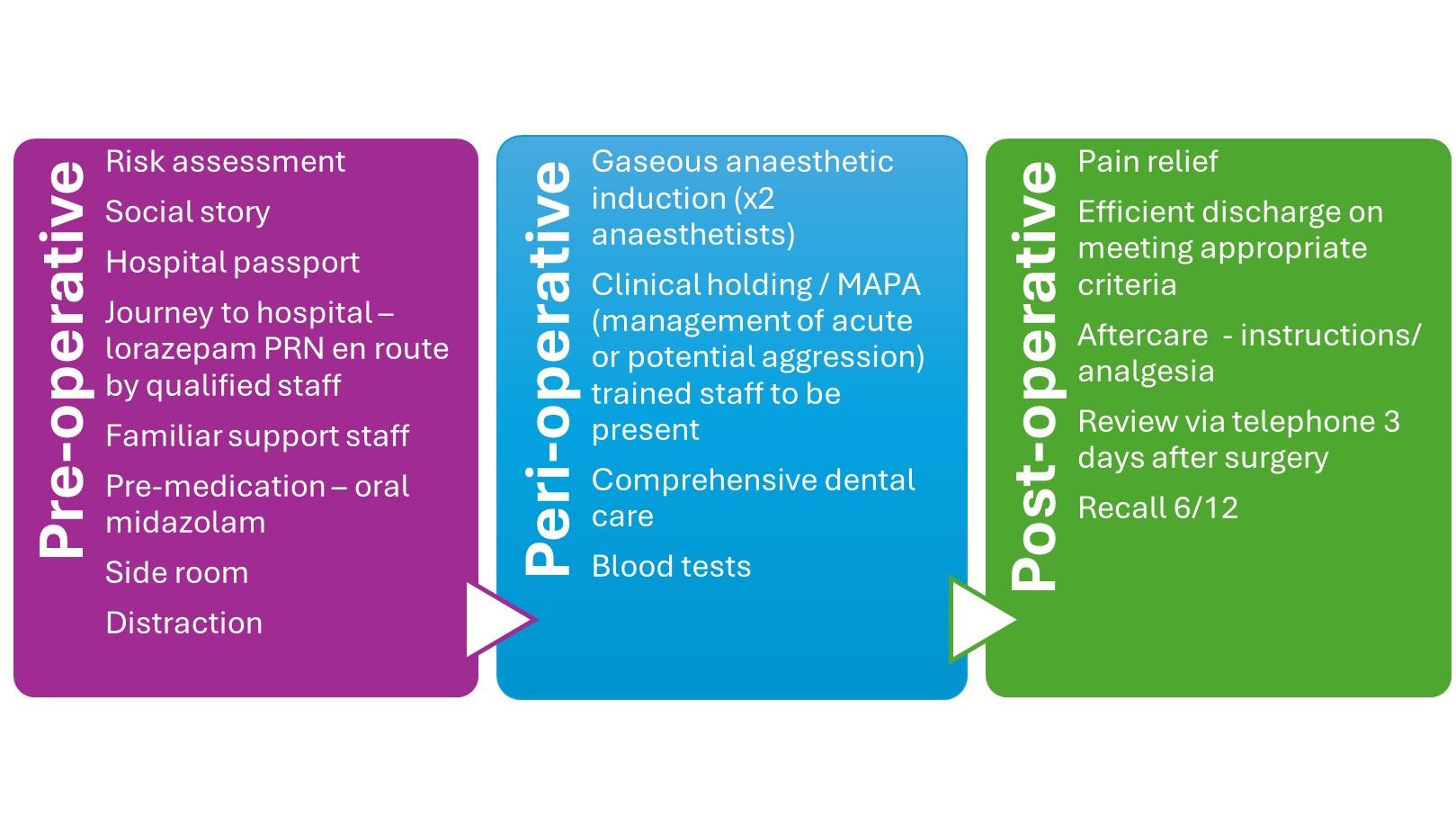
Fig 3. Reasonable adjustments made to facilitate comprehensive dental treatment
Long term treatment and future considerations
The dental treatment under GA was undertaken by two clinicians in agreement with the above plan,4 thereafter the patient was deemed dentally fit. Whilst there was a significant time period required to plan appropriately, during which the patient’s oral health deteriorated; once the planned treatment modality was confirmed, the GA dental treatment date was expedited as the patient was planned to be stepped down into community living facilities. It was predicted that he would be likely to have less support (medically and psychologically) upon step-down and therefore it was important that his dental condition be managed prior to this.
Due to his continued high caries and periodontal risk, measures in line with Delivering Better Oral Health5 were undertaken regarding oral hygiene instruction, diet advice and fluoride therapy to prevent future deterioration of his dental condition with a three- month recall interval.
Meeting the patient within his own environment during the domiciliary visit allowed rapport to be built with the clinicians and discussion of his fear and anxiety around dentists which was specifically due to a needle phobia. Following stabilisation of his dental condition, it was considered that cognitive behavioural therapy may be an appropriate future consideration to manage his needle phobia and allow easier access to dental care in the future.
Discussion and reflection about case presented
The timeline of this case spans over a year, after initial missed appointments, engagement with the patient’s medical team through case discussion was necessary to plan subsequent steps.
Whilst initially intravenous sedation was considered, it was likely that a bolus oral dose / intranasal sedation would be required to allow cannulation which was deemed unsafe due to the patient’s high BMI. Anaesthetic opinion following initial consultation allowed for direction towards the safest treatment modality.
Involvement of the patient’s family was crucial in gaining a background into the patient’s needle phobia, family members also attended on the day of surgery to support his care.
Through close communication with IMHSU, we understood the risks and challenges presented by the patient and co-ordinated a social story to aid familiarity with the environment prior to surgery alongside a hospital passport which aided in hospital staff understanding his needs prior to surgery.
This case highlights the challenges in managing patients with dental need and enduring mental health conditions, medical co-morbidities and who lack capacity.
The dental team took a proactive approach to identify and understand the needs of this patient and brought together the right team to achieve a reduction in the barriers and facilitate a successful outcome. Multidisciplinary team (MDT) approach with close co-ordination between medical, dental and mental health teams allowed for safe provision of the dental treatment under GA. The time and planning involved was extremely valuable and essential in the success of this patient’s management and provides a framework for improving healthcare access for future complex cases.
Acknowledgements
Thank you to the anaesthetic, vulnerabilities and ambulatory care team at the Queen Elizabeth Hospital, Birmingham and the nursing staff, support workers and psychiatry team at the Gerry Simon Unit for aiding in facilitating this patient’s care.
Conflict of interest
The author declares that there is no conflict of interest.
References
1. Chung F, Abdullah H R, Liao P. STOP-Bang Questionnaire: A Practical Approach to Screen for Obstructive Sleep Apnea, Chest 2016; 149: 3, 631-638. DOI: 10.1378/chest.15-0903
2. Office of the Public Guardian. Mental Capacity Act Code of Practice. 2013. Online information available at: https://www.gov.uk/government/publications/mental-capacity-act-code-of-practice (Accessed October 2024).
3. British Society for Disability and Oral Health. Guidelines for ‘Clinical Holding’ Skills for Dental Services for people unable to comply with routine oral health care. 2009. https://www.bsscd.org/index.php/component/edocman/bsdh-clinical-holding-guideline-jan-2010-pdf?Itemid=0 (Accessed October 2024)
4. Geddis-Regan A R, Gray D, Buckingham S, Misra U, Boyle C. The use of general anaesthesia in special care dentistry: A clinical guideline from the British Society for Disability and Oral Health. Spec Care Dentist. 2022; 42: 3–32. DOI: 10.1111/scd.12652
5. Office for Health Improvement and Disparities, Department of Health and Social Care, NHS England and NHS Improvement. Delivering better oral health: an evidence-based toolkit for prevention. 2014. Online information avalable at: https://www.gov.uk/government/publications/delivering-better-oral-health-an-evidence-based-toolkit-for-prevention (Accessed October 2024).

