Please click on the tables and figures to enlarge
Improving safety and efficiency in special care dentistry through quality improvement of patient information in the Belfast Trust
L. Cullen*1 BDS, PGCertClinEd
K. McKenna2 BDS, MFDS, DSCD, PGcertClinEd, MSCD
1Dental Core Trainee in Special Care Dentistry, Royal School of Dentistry, Belfast Health and Social Care Trust
2Locum Consultant in Special Care Dentistry, Royal School of Dentistry, Belfast Health and Social Care Trust
*Correspondence to: Louise Cullen
Email: louise.cullen@belfasttrust.hscni.net
Cullen L, McKenna K. Improving safety & efficiency in special care dentistry through quality improvement of patient information in the Belfast Trust. SAAD Dig. 2024: 40(1): 15-18
Abstract
The Belfast Health and Social Care Trust’s Special Care Dentistry unit provides treatment under conscious sedation and general anaesthetic. Patients were sent generic preoperative information which was not in a user friendly format for special care dentistry. This presented a patient safety issue with reliance on staff to verbally reinforce information.
Through a quality improvement project we aimed to design a new patient information leaflet to improve safety and clinical effectiveness; incorporate guidance and reduce variation; improve patient experience and improve efficiency within our service by reducing staff administration time.
Plan Do Study Act (PDSA) cycles collated information from dental trainees, nurses and patients. Patient and carer feedback was sought on the quality and usefulness of information. We utilised patient feedback and a reading group to develop a new special care dentistry preoperative information leaflet.
Through quality improvement and service user engagement we have improved patient safety and satisfaction and improved efficiency through the standardisation of pre-operative information.
Introduction
The Special Care Dentistry (SCD) Department at the Belfast Health and Social Care Trust provides a dental service for patients who have significant physical, sensory, mental, emotional or social impairment or disability. Referrals are received from general dental practitioners, the community dental service and other hospital dental service departments. Dental treatment is provided under local anaesthetic with additional monitoring, conscious sedation or general anaesthesia in our day procedure unit, or as inpatients when required.
New patients receive multidisciplinary team assessment, with anaesthetic support. In addition to the clinical assessment and special investigations, a detailed discussion of dental treatment and treatment modality options is undertaken. Patients are given verbal pre- and post-operative instructions. These instructions are reinforced with a generic patient information sheet which they receive with the treatment appointment letter.
Tailored individual instructions are provided, if required, to reduce the risk of complications both peri- and post-operatively with the primary aim of ensuring patient safety.
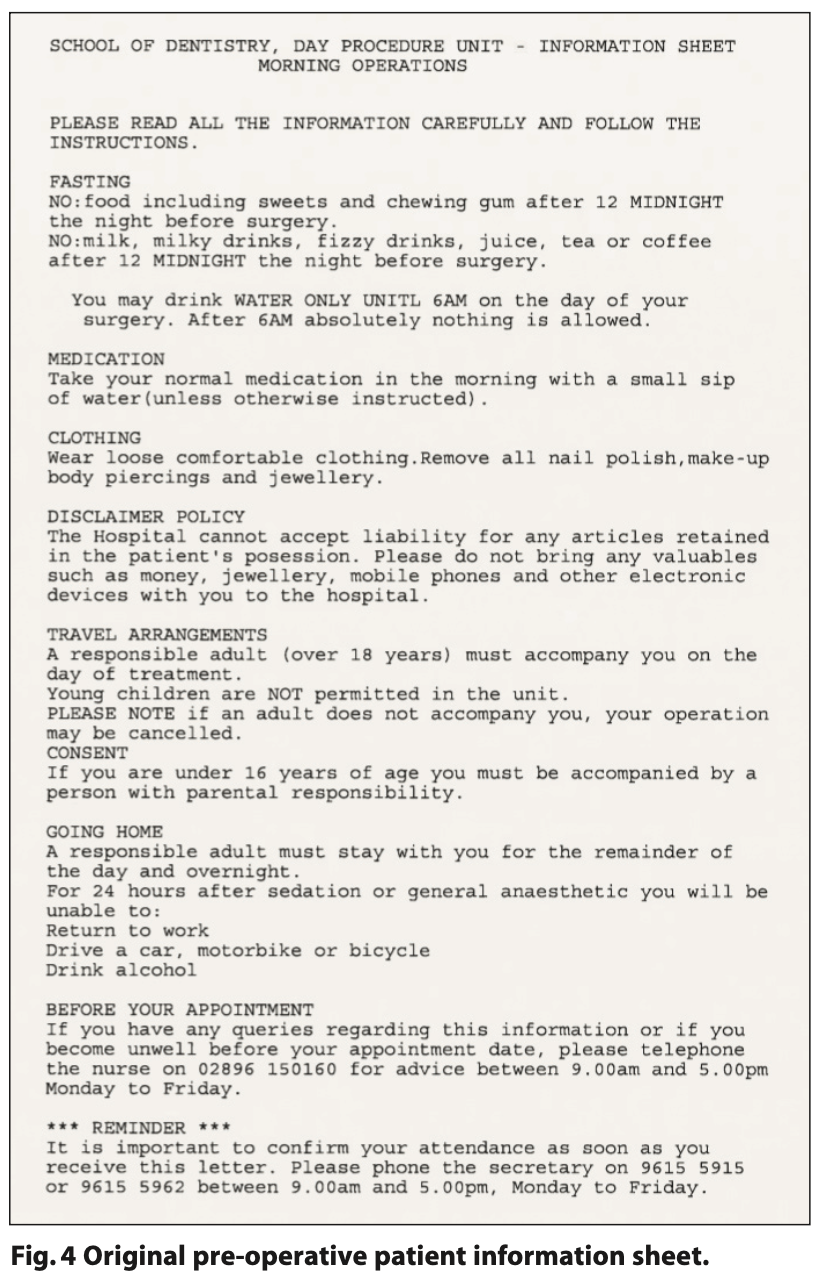
We noted anecdotal evidence that the generic written pre- operative information being used in our department was not user- friendly (Figure 4), with frequent calls from patients and carers to clarify instructions, in particular fasting instructions. This presented a patient safety issue, relying on Dental Core Trainees (DCT) and nursing staff to contact each patient to verbally reinforce the pre-operative information prior to the procedure. This presented a high administrative burden with heavy reliance on individual staff members. There was duplication of work, with unclear roles and responsibilities, as both dental core trainees and nursing colleagues assumed this role.
Quality improvement (QI) is ‘…a systematic approach to improving service quality, efficiency and morale’.1 The Model for Improvement advocated by quality improvement initiatives aims to achieve improvements in healthcare systems, processes and outcomes using a standardised methodology which includes the implementation of Plan Do Study Act (PDSA) cycles to test changes, while continually monitoring data to assess for improvements in performance.2
Prioritising QI will help our service to optimise patient outcomes and safety and promote a patient-centred approach. The concept of ‘patient-centred care’ is fundamental to SCD. Promotion and engagement with QI is particularly important within SCD, because, as the most recently established of the dental specialities, there is a lack of evidence-based resource to support interventions.
The definition we used for quality was derived from the ‘Quality 2020’ initiative which is a ten year strategy to improve health and social care in Northern Ireland.3 This strategy defines quality under three domains of safety, effectiveness and patient and client focus.
Aims
We aimed to employ an evidence-based approach to QI, by designing a new patient information leaflet to improve the quality of the pre-operative information; maintain patient satisfaction and to achieve full compliance with the fasting instructions in the absence of the pre-operative phone call therefore reducing staff administration time and promoting a more efficient service.
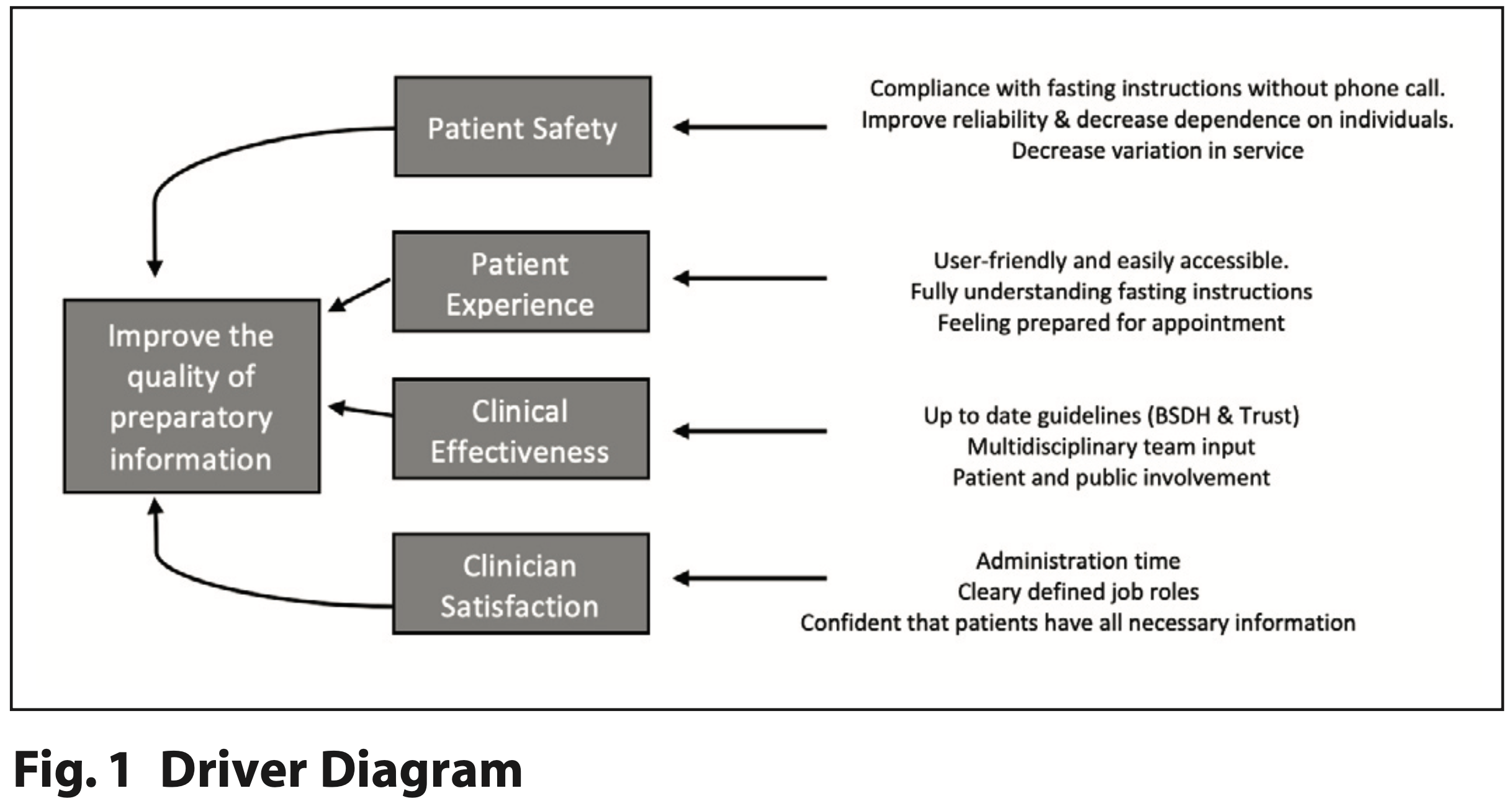
By improving the quality of the pre-operative information, we aimed to improve:
- Patient safety by reducing variation in information given and building resilience into the system by reducing dependence on staff
- Clinical effectiveness by incorporating recent evidence- based guidance
- Patient experience by involving patients
- Efficiency within the department by reducing staff administration time.
(See Figure 1).
These aims are central to the ten-year strategy to improve quality in Health and Social Care in Northern Ireland entitled ‘Quality 2020’. This strategy defines quality under three domains of:
- Safety, avoiding and preventing harm to patients and clients from the care, treatment and support that is intended to help them
- Effectiveness, the degree to which each patient and client receives the right care (according to scientific knowledge and evidence-based assessment), at the right time in the right place, with the best outcome and finally
- Patient and client focus, all patients and clients are entitled to be treated with dignity and respect and should be fully involved in decisions affecting their treatment, care and support.3
Methodology
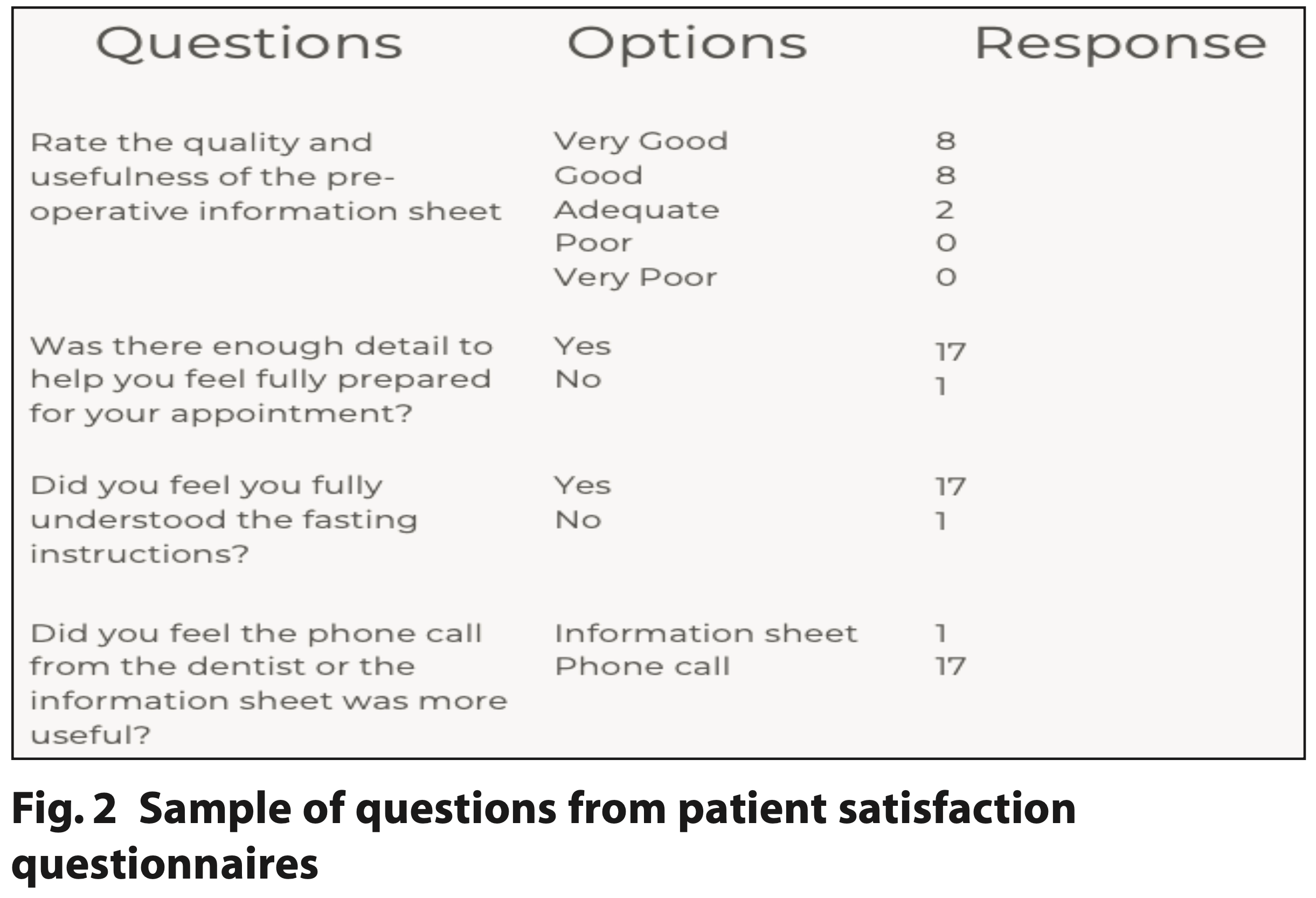
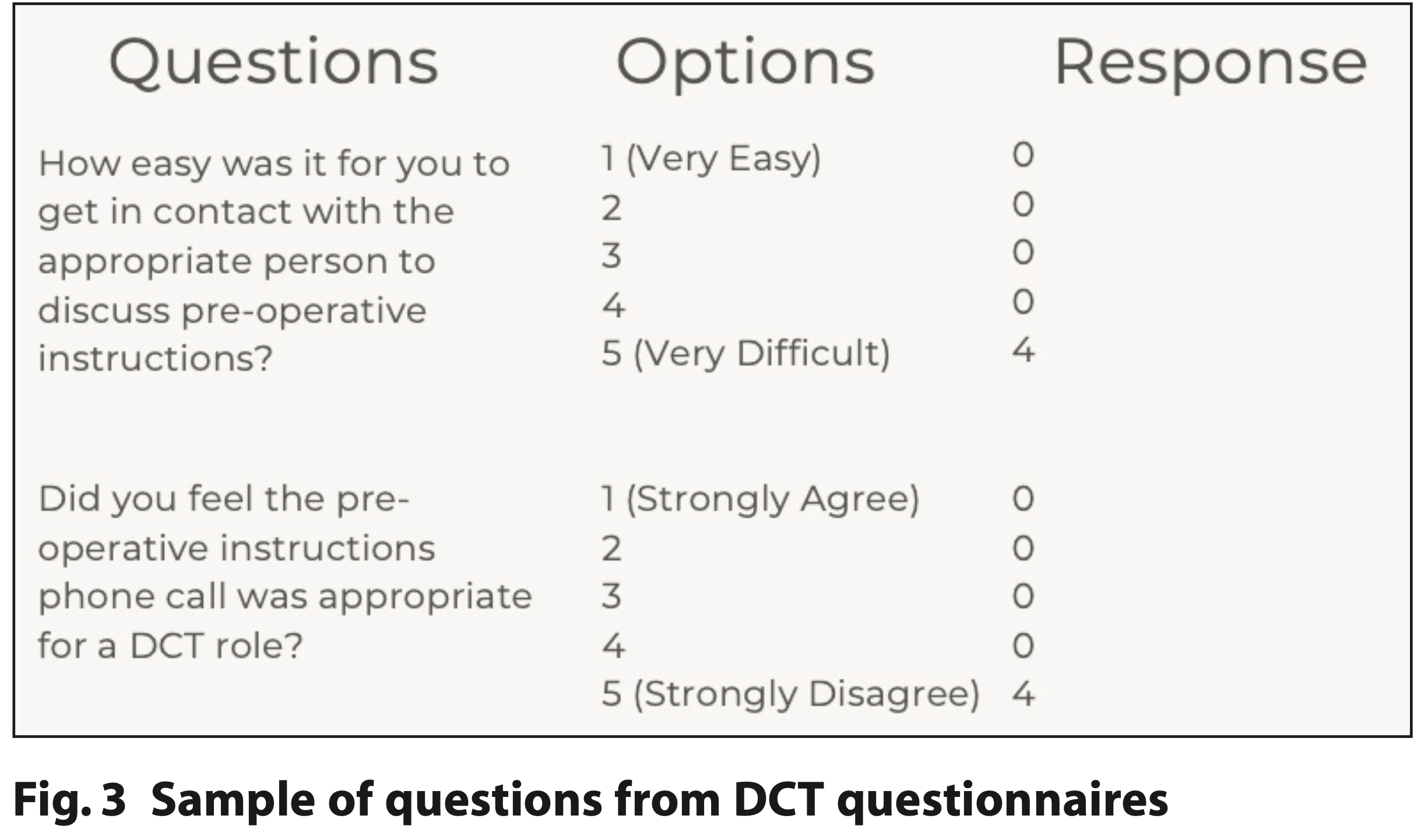
A prospective QI project with two PDSA cycles was carried out within the SCD department. PDSA cycles collated questionnaire information from DCTs, nurses and patients (see Figures 2 and 3). We used feedback and a patient / carer reading group to develop a new SCD preoperative information leaflet. PDSA cycle one was conducted from November 2021 to February 2022 and PDSA cycle two from April to July 2022.
Recommendations were made and implemented between cycles. Information was collated from staff working in the department and patients / carers. In both cycles, a survey was distributed to all Dental Core Trainees working within the SCD department to quantify time spent on pre-operative patient preparation and qualitative feedback regarding clarity of roles and responsibilities within the department. Additionally, patient feedback was collated through written satisfaction questionnaires which were distributed to patients and carers when they attended for their dental sedation / general anaesthetic appointment.
Results
PDSA cycle one
In cycle one, staff spent on average 42 minutes per theatre session completing pre-operative phone calls. Eighteen patients who completed the satisfaction questionnaire, 94% (n = 18) found the pre-operative phone call more useful than the leaflet.
Within the SCD department we held a multidisciplinary team meeting with dental, anaesthetic and nursing colleagues to discuss the results of these questionnaires and define roles and responsibilities. This was implemented with the pilot of the new patient information leaflet. Staff would no longer be completing the pre-operative phone call. A multidisciplinary collaborative approach was utilised to co-design a new patient information leaflet.
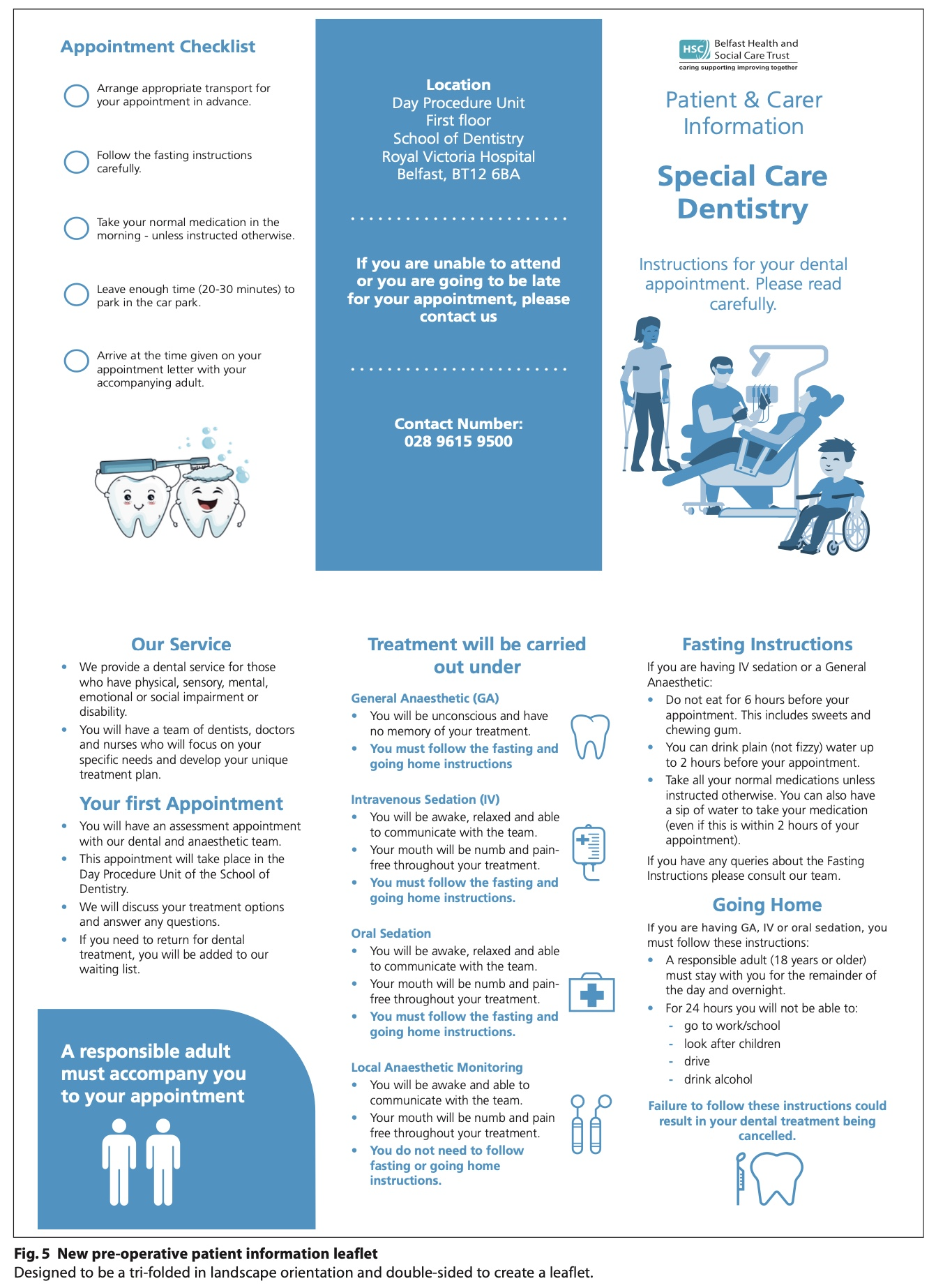
The NHS Toolkit for Producing Patient Information provided guidance on how to ensure the details are inclusive and patient friendly eg ensuring short sentences (15 to 20 words), use of everyday language (avoiding jargon), question and answer format and patient-friendly text (including the use of personal pronouns ie, ‘we’ and ‘you’).4
As part of the clinical governance framework, ensuring patient and public involvement to achieve patient-centred improvements in our service is essential. The initial draft of the new patient information leaflet was submitted to the Trust’s panel for feedback to ensure the information provided was ‘…informative, easy to understand, makes sense and answers the questions people might have.’ 5
This feedback highlighted the importance of ensuring language was simple and instructions were clear and concise. The Government’s 2011 Skills for Life Survey found that 43% of English adults aged 16 to 65 years had literacy skills lower than those expected of a 13 to 14-year-old child.6 The reading panel also highlighted the potential for confusion with the fasting instructions with regards to the use of liquids to take medication before the appointment, especially for an early morning appointment. This prompted a further redraft and inclusion of specific instructions on taking medications.
Additionally, our patients and their carers can have high levels of anxiety in respect of their dental treatment. This can influence their interpretation of, and compliance with, the patient instructions. It was important to consider that the information was delivered in an appropriate manner to avoid increasing patient anxiety. Following a redraft of the information leaflet, we piloted the new information leaflet within our department over a six-week period (see Figure 5). As before, verbal instructions were given at the assessment visit, with instructions reinforced in writing using the new patient information leaflet which was sent with the appointment letter.
Following the six-week pilot we collected another set of patient and staff satisfaction questionnaires.
PDSA cycle two
In cycle two, staff administration time fell to nine minutes per theatre session and 100% of patients found the new information leaflet to be more user-friendly.
Conclusion
Pre-operative information is vital to ensure patient safety and maintain professional standards.
Through an evidence-based approach to QI we have standardised the pre-operative information, redefined staff roles and responsibilities, improved patient safety and satisfaction and improved the efficiency of our service.
Staff administration time was significantly reduced (80%), and patient and staff satisfaction increased (15%), with full patient compliance with written fasting instructions.
By improving the quality of written patient information we have noted improvements for:
- Patients: improved satisfaction with pre-operative information in quality, presentation and usefulness
- Staff: administration time reduced by 80%, with improved job satisfaction, and clarity of roles and responsibilities. No longer duplication of work between DCTs and nursing teams
- Trust: improved quality of service by improving clinical effectiveness and patient safety, standardising information to reduce variation in the standard of care, improved resilience in the system by reducing reliance on individuals and ensuring service user engagement through patient and public involvement.
These improvements have enhanced the quality of our service. However, we acknowledge that the project was limited by the resources available. The development of new technologies, such as digital formats and QR codes, has created the opportunity to increase patient engagement and improve the dissemination of information. Introducing a digital leaflet with audio and video clips could greatly benefit patients with additional needs by providing clearer explanations of procedures and instructions. Quality improvement is ongoing within the SCD department and we continue to explore innovative solutions to optimise patient outcomes, satisfaction and the quality of care.
Declaration of Interest
There are no conflicts of interest.
References
1. NHS. Service improvement and transformation. Online information available at https://www.england.nhs.uk/mat-transformation/matrons-handbook/service-improvement-and-transformation/
2. QI Essentials Toolkit. Institute for Health Improvement, 2017.
3. 10-year strategy to protect and improve quality in health and social care in Northern Ireland. Department of Heath, Social Care and Public Services. 2020.
4. Department of Health. Toolkit for Producing Patient Information. London: DH; 2003.
5. Cause. Reading Panel. 2022. Online information available at https://www.cause.org.uk/news/interested-in-joining-bhsct-reader-panel
6. Department for Business Innovation and Skills. The 2011 Skills for Life Survey: A Survey of Literacy, Numeracy and ICT Levels in England. London: BIS, 2012.